Whether you’re documenting a client’s symptoms or preparing a treatment plan, knowing the correct ICD-10 code for Alcohol Use Disorder (AUD) is essential for accurate diagnosis, billing, and continuity of care.
This guide walks you through the 2025 ICD-10 codes for Alcohol Use Disorder, explains key diagnostic criteria, and offers practical tips for clear, defensible documentation — especially when working with insurance or compliance audits.
Yet even with the right codes in hand, many clinicians find it challenging to justify a diagnosis clearly in their notes, particularly when connecting observed symptoms to ICD-10 criteria.
That’s where Mentalyc helps. As a clinical intelligence platform, it automatically captures relevant symptoms and progress patterns from your sessions — helping you document diagnostic reasoning clearly, confidently, and in full compliance.

New! Transfer your notes to EHR with a single click. No more copy-pasting.
Alcohol Use Disorder: What Are We Talking About?
Alcohol use disorder (AUD) is a complex medical condition, marked by a concerning inability to rein in or manage alcohol consumption despite the looming threat of adverse social, occupational, and health repercussions.
It encompasses a spectrum of issues, from what some folks casually refer to as alcohol abuse or alcohol dependence, to the more down-to-earth term, alcoholism. Understanding this condition in clinical terms often involves identifying the appropriate ICD-10 code for Alcohol Use Disorder to ensure accurate diagnosis and treatment documentation. AUD can come in three level: mild, moderate, or a full-blown severe case.
When Does Drinking Become Alcohol Use Disorder?
In clinical practice, the line between social drinking and Alcohol Use Disorder (AUD) is defined not by quantity alone, but by the functional impact and loss of control over consumption. While public health guidelines describe “moderate use” (up to two drinks daily for men and one for women), therapists focus on patterns that indicate impaired functioning, tolerance, or withdrawal.
AUD is diagnosed when drinking behavior leads to clinically significant distress or impairment, such as repeated work absences, strained relationships, risky behaviors, or inability to reduce intake despite consequences. Over time, clients may show increased tolerance or withdrawal symptoms, which are critical diagnostic markers under the DSM-5 and ICD-10 criteria.
Understanding these distinctions helps clinicians determine whether a client meets the threshold for an AUD diagnosis, guiding both treatment planning and accurate ICD-10 coding.
How to Detect Alcohol Use Disorder?
Recognizing such a condition involves identifying a range of concerning behaviors and symptoms in patients.
Common Signs and Symptoms of Alcohol Use Disorder (AUD)
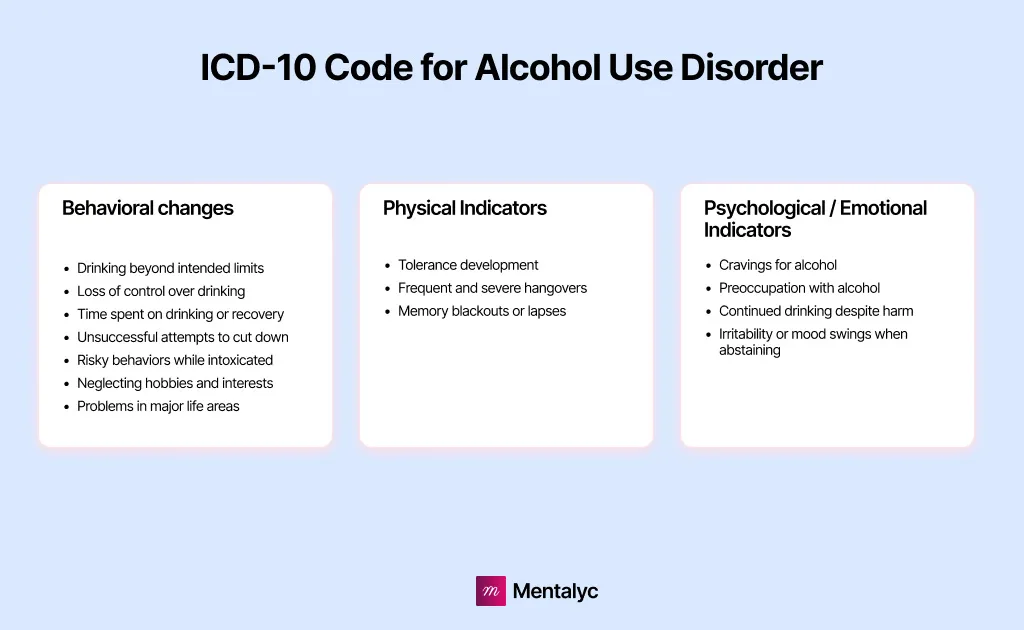
| # | Sign or Symptom | Clinical Description |
| 1 | Memory blackouts or lapses | The client reports episodes of amnesia or memory gaps after drinking. |
| 2 | Continued drinking despite harm | Alcohol use persists even when it causes distress or harm to oneself or others. |
| 3 | Drinking beyond intended limits | The individual consumes more alcohol or drinks longer than initially planned. |
| 4 | Irritability or mood swings when abstaining | The client exhibits irritability, restlessness, or anxiety when not drinking. |
| 5 | Frequent and severe hangovers | Recurrent episodes of fatigue, nausea, or physical discomfort following drinking. |
| 6 | Risky behaviors while intoxicated | Includes drunk driving, unsafe sex, or other dangerous actions under the influence. |
| 7 | Neglecting hobbies and interests | Activities once enjoyed are abandoned to prioritize alcohol use. |
| 8 | Cravings for alcohol | Strong urges or obsessive thoughts about drinking. |
| 9 | Problems in major life areas | Alcohol-related issues repeatedly affect work, school, relationships, or legal standing. |
| 10 | Tolerance development | Increasing amounts of alcohol are required to achieve the same effects. |
| 11 | Loss of control over drinking | The client struggles to stop drinking once they’ve started. |
| 12 | Time spent on drinking or recovery | A significant portion of the day is devoted to drinking or recovering from hangovers. |
| 13 | Unsuccessful attempts to cut down | The person expresses a desire to reduce intake but cannot maintain abstinence. |
| 14 | Preoccupation with alcohol | Alcohol becomes a central focus in daily life, overshadowing responsibilities or goals. |
Common Symptoms of Alcohol Withdrawal
Furthermore, individuals with alcohol use disorder may encounter withdrawal symptoms when attempting to reduce or cease their alcohol intake, which can encompass:
| # | Symptom | Clinical Description |
| 1 | Anxiety | Persistent feelings of nervousness, tension, or unease during early withdrawal. |
| 2 | Depressive episodes | Low mood, hopelessness, or loss of interest often emerging as alcohol levels drop. |
| 3 | Irritability | Heightened sensitivity or anger during withdrawal; emotional volatility is common. |
| 4 | Nausea and dry heaving | Gastrointestinal distress that may persist for several days post-cessation. |
| 5 | Rapid heart rate | Elevated pulse or palpitations caused by nervous system hyperactivity. |
| 6 | Restlessness | Inability to sit still or relax, often paired with agitation or racing thoughts. |
| 7 | Tremors or shakiness | Noticeable trembling of the hands or body, especially in the morning. |
| 8 | Profuse sweating | Excessive perspiration, particularly at night or during early detox. |
| 9 | Sleep disturbances | Insomnia, vivid dreams, or frequent waking throughout the night. |
| 10 | Seizures | Convulsive episodes due to severe withdrawal or unmanaged detox. |
| 11 | Hallucinations | Seeing or hearing things that are not real, often within 12–24 hours of cessation. |
| 12 | Delirium tremens (DTs) | A severe withdrawal reaction involving confusion, disorientation, and agitation. |
| 13 | Coma or death (in extreme cases) | Life-threatening complications that require immediate medical intervention. |
Clinicians assessing these symptoms often refer to the ICD-10 codes for alcoholism to accurately document the diagnosis and guide evidence-based treatment.
Now, if we want to be more precise, healthcare professionals rely on the Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5) criteria to evaluate whether an individual exhibits symptoms of Alcohol Use Disorder (AUD) and to gauge the disorder’s severity, should it be present.
Severity is gauged based on the number of criteria a person meets in relation to their symptoms, categorized as Mild Moderate Severe Alcohol Use Disorder — mild (2–3 criteria), moderate (4–5 criteria), or severe (6 or more criteria).
DSM-5 Criteria for Alcohol Use Disorder Severity
| Severity Level | Number of DSM-5 Criteria Met | Clinical Description | Example Presentation |
| Mild Alcohol Use Disorder | 2–3 criteria | Early-stage problematic drinking; minimal physiological dependence. | Client occasionally drinks more than intended or experiences mild consequences. |
| Moderate Alcohol Use Disorder | 4–5 criteria | Clear pattern of impaired control, risky use, and social/interpersonal issues. | Client continues drinking despite job or relationship issues; shows tolerance. |
| Severe Alcohol Use Disorder | 6 or more criteria | Significant physical dependence, withdrawal, and life disruption. | Client prioritizes alcohol over all other responsibilities and shows withdrawal symptoms when abstinent. |
Alcohol Use Disorder (AUD) Screening Questions
To assess a person’s symptoms, you might pose the following questions to your client. These questions not only help determine the presence of AUD but also guide clinicians in applying the correct alcohol addiction diagnosis codes, ensuring consistency in clinical documentation and insurance billing.
| # | Screening Question | What It Assesses |
| 1 | Have you found yourself drinking more or for a longer duration than you originally intended? | Evaluates loss of control over drinking quantity or duration. |
| 2 | Have you tried to cut down or stop drinking but were unable to do so despite wanting to? | Assesses unsuccessful attempts to reduce or stop alcohol use. |
| 3 | Have you spent a significant amount of time drinking, recovering from drinking, or dealing with its aftereffects? | Identifies time investment and interference with daily functioning. |
| 4 | Have you experienced strong cravings or urges to drink? | Measures psychological dependence and intensity of alcohol craving. |
| 5 | Has drinking or being hungover interfered with work, school, home, or family responsibilities? | Examines impairment in major life areas due to alcohol use. |
| 6 | Have you continued drinking despite ongoing problems with family or friends? | Evaluates continued use despite interpersonal or social consequences. |
| 7 | Have you given up or reduced activities you once enjoyed because of drinking? | Indicates neglect of important activities and behavioral shifts. |
| 8 | Have you put yourself in risky situations while drinking, such as driving, swimming, using machinery, or engaging in unsafe sex? | Assesses risky behaviors and impaired judgment under intoxication. |
| 9 | Have you kept drinking even though it worsened depression, anxiety, or other health problems? | Measures continued use despite physical or psychological harm. |
| 10 | Have you noticed you need more alcohol to feel its effects, or that the same amount has less effect than before? | Screens for tolerance, a key physiological marker of dependence. |
| 11 | When the effects of alcohol wear off, do you experience withdrawal symptoms such as tremors, nausea, sweating, anxiety, or hallucinations? | Detects withdrawal symptoms and physiological dependence. |
Stages of Alcohol Use Disorder: From At-Risk to End-Stage
Well, it turns out that the journey from casual drinking to a full-blown addiction is a rollercoaster ride.
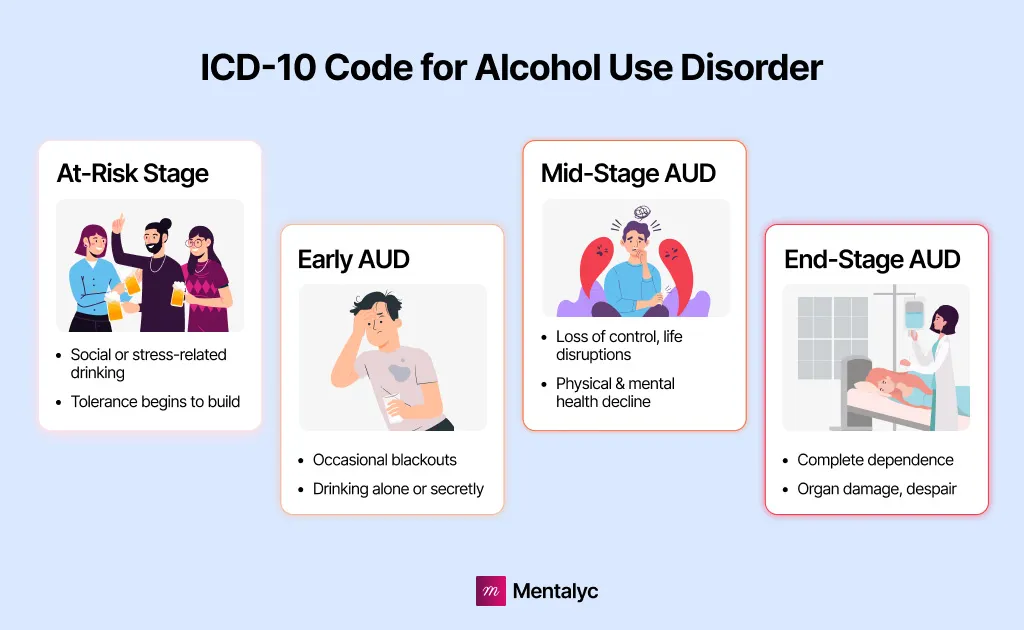
1. The At-risk Stage:
Picture this: you’re out with your friends, enjoying a few drinks, or maybe you’ve had a rough day at work, and a glass of wine seems like the perfect way to unwind. It all starts innocently enough. You might even find yourself reaching for that bottle a bit more often. It’s in this phase that you’re walking on the edge. You’re either sipping for social kicks or seeking solace in that drink, thinking it’s the answer to your problems. And you know what’s sneaking in? Tolerance. Your body’s getting used to the booze.
2. The Early Alcohol Use Disorder:
Now, things are starting to take a darker turn. Blackouts become your not-so-friendly companions, and you’re not just having a drink for fun anymore. In fact, you might be sneaking off to have a few alone or keeping it hush-hush. The alcohol is slowly but surely seeping into your thoughts more often. It’s creeping into your life.
3. The Mid-Stage Alcohol Use Disorder:
This is when you’ve lost the reins. Your alcohol use has gone haywire, and it’s dragging your life down with it. Work? Family? Finances? Your physical and mental health? They’re all taking hits. It’s not just about getting tipsy anymore; it’s about getting control. And here’s the scary part – lab tests and scans start showing signs of the damage. Your body is crying out, but you can’t hear it over the clinking of glasses. This progression is often where providers formally document alcohol use disorder symptoms and diagnosis to capture the growing severity.
4. The End-Stage Alcohol Use Disorder:
Welcome to the darkest chapter. Alcohol is no longer a part of your life; it’s your entire life. You’ve traded in food, intimacy, health, and happiness for that drink. The bottle becomes your only solace, and nothing else matters. Despair is your constant companion and complications from organ damage are knocking on your door. Death? Well, it’s lurking in the shadows.
In these severe cases, clinicians rely on precise alcohol use disorder treatment coding and DSM-based criteria to ensure that treatment planning, documentation, and intervention reflect the true complexity of the client’s condition.
ICD-10 Codes for Alcohol Use Disorder (With Examples)
Below, we gathered all Alcohol Use Disorder ICD-10 codes related to alcohol abuse, dependence, and associated disorders. This table should serve as a valuable reference to facilitate professionals’ lives, enabling them to precisely categorize and address alcohol-related disorders ICD-10 in patient records.
ICD-10 Codes for Alcohol Use Disorder (Quick Reference)
| Code | Description |
| F1010 | Alcohol abuse, uncomplicated |
| F1011 | Alcohol abuse, in remission |
| F10120 | Alcohol abuse with intoxication, uncomplicated |
| F10121 | Alcohol abuse with intoxication delirium |
| F10129 | Alcohol abuse with intoxication, unspecified |
| F1014 | Alcohol abuse with alcohol-induced mood disorder |
| F10150 | Alcohol abuse with alcohol-induced psychotic disorder with delusions |
| F10151 | Alcohol abuse with alcohol-induced psychotic disorder with hallucinations |
| F10159 | Alcohol abuse with alcohol-induced psychotic disorder, unspecified |
| F10180 | Alcohol abuse with alcohol-induced anxiety disorder |
| F10181 | Alcohol abuse with alcohol-induced sexual dysfunction |
| F10182 | Alcohol abuse with alcohol-induced sleep disorder |
| F10188 | Alcohol abuse with other alcohol-induced disorder |
| F1019 | Alcohol abuse with unspecified alcohol-induced disorder |
| F1020 | Alcohol dependence, uncomplicated |
| F1021 | Alcohol dependence, in remission |
| F10220 | Alcohol dependence with intoxication, uncomplicated |
| F10221 | Alcohol dependence with intoxication delirium |
| F10229 | Alcohol dependence with intoxication, unspecified |
| F10230 | Alcohol dependence with withdrawal, uncomplicated |
| F10231 | Alcohol dependence with withdrawal delirium |
| F10232 | Alcohol dependence with withdrawal with perceptual disturbance |
| F10239 | Alcohol dependence with withdrawal, unspecified |
| F1024 | Alcohol dependence with alcohol-induced mood disorder |
| F10250 | Alcohol dependence with alcohol-induced psychotic disorder with delusions |
| F10251 | Alcohol dependence with alcohol-induced psychotic disorder with hallucinations |
| F10259 | Alcohol dependence with alcohol-induced psychotic disorder, unspecified |
| F1026 | Alcohol dependence with alcohol-induced persisting amnestic disorder |
| F1027 | Alcohol dependence with alcohol-induced persisting dementia |
| F10280 | Alcohol dependence with alcohol-induced anxiety disorder |
| F10281 | Alcohol dependence with alcohol-induced sexual dysfunction |
| F10282 | Alcohol dependence with alcohol-induced sleep disorder |
| F10288 | Alcohol dependence with other alcohol-induced disorder |
| F1029 | Alcohol dependence with unspecified alcohol-induced disorder |
| F10920 | Alcohol use, unspecified with intoxication, uncomplicated |
| F10921 | Alcohol use, unspecified with intoxication delirium |
| F10929 | Alcohol use, unspecified with intoxication, unspecified |
| F1094 | Alcohol use, unspecified with alcohol-induced mood disorder |
| F10950 | Alcohol use, unspecified with alcohol-induced psychotic disorder with delusions |
| F10951 | Alcohol use, unspecified with alcohol-induced psychotic disorder with hallucinations |
| F10959 | Alcohol use, unspecified with alcohol-induced psychotic disorder, unspecified |
| F1096 | Alcohol use, unspecified with alcohol-induced persisting amnestic disorder |
| F1097 | Alcohol use, unspecified with alcohol-induced persisting dementia |
| F10980 | Alcohol use, unspecified with alcohol-induced anxiety disorder |
| F10981 | Alcohol use, unspecified with alcohol-induced sexual dysfunction |
| F10982 | Alcohol use, unspecified with alcohol-induced sleep disorder |
| F10988 | Alcohol use, unspecified with other alcohol-induced disorder |
| F1099 | Alcohol use, unspecified with unspecified alcohol-induced disorder |
ICD-10 Coding Example for Alcohol Use Disorder
A 58-year-old gentleman, whom we shall refer to as Mr. M, arrived at the primary care provider’s office, voicing concerns about anxiety. During the course of an in-depth conversation with this patient, the healthcare provider began to gain a deeper understanding of Mr. M’s relationship with alcohol. It became evident that the challenges brought about by the last COVID-19 pandemic had taken a toll on Mr. M’s small business. Under the weight of financial stress, he acknowledged a gradual escalation in his alcohol consumption.
Upon further exploration, the provider uncovered that Mr. M had made attempts to quit drinking but had been unsuccessful, experiencing the aftermath of several hangovers.
Family members had recently expressed their concerns about his drinking habits. Remarkably, even in the face of heightened anxiety, Mr. M continued to engage in drinking, fully aware of its detrimental effects. He also disclosed that his relationship with his spouse had become more strained. Notably, he denied experiencing alcohol withdrawal ICD-10 symptoms, such as sleep disturbances, tremors, restlessness, nausea, perspiration, palpitations, or seizures.
Considering the criteria set forth in the DSM-5, it appears that Mr. M could be diagnosed with Mild Alcohol Use Disorder, as indicated by the ICD-10 code for Alcohol Use Disorder F10.10.
Looking ahead, if Mr. M returns for a follow-up in six weeks and his alcohol consumption persists or intensifies rather than abating, he may meet the criteria for a diagnosis of Moderate Alcohol Use Disorder or even Alcoholism, marked by the Alcohol dependence ICD-10 code F10.20. Such a diagnosis would place Mr. M at an elevated risk for various concurrent health issues, including mental health challenges, cardiovascular problems, liver disease, pancreatic inflammation, and others — consistent with broader patterns seen in alcohol abuse ICD-10 cases.
Document AUD Cases with Confidence and Clarity
Accurately coding and documenting Alcohol Use Disorder (AUD) takes more than memorizing ICD-10 numbers. It’s about capturing the nuances of each client’s symptoms, progress, and recovery story in a defensible way.
With Mentalyc, therapists can automatically surface relevant symptoms and track client progress over time, making diagnostic reasoning clear and audit-ready. It’s documentation that supports your clinical judgment, strengthens compliance, and helps you stay focused on what matters most — your clients’ healing.
Try Mentalyc today and experience how you can make ICD-10 documentation simpler, sharper, and more defensible.
Frequently Asked Questions (FAQs) About ICD-10 Code for Alcohol Use Disorder (AUD)
1. What Is Alcohol Use Disorder (AUD)?
Alcohol Use Disorder (AUD) is a chronic, relapsing brain condition characterized by an impaired ability to stop or control alcohol use despite harmful consequences. According to the DSM-5 Alcohol Use Disorder definition, it encompasses a spectrum of severity—mild, moderate, and severe—based on the number of symptoms present. AUD affects both the brain and body, leading to physical dependence, tolerance, and emotional distress when alcohol is unavailable.
2. When Does Drinking Become Alcohol Use Disorder?
Drinking transitions into a diagnosable disorder when alcohol consumption leads to significant impairment or distress in daily functioning. This includes relationship problems, work or academic decline, and health complications. Clinicians use standardized tools and the DSM-5 criteria for Alcohol Use Disorder to determine whether drinking patterns meet the threshold for diagnosis, moving from occasional use to dependency.
3. What Are the Signs and Symptoms of Alcohol Use Disorder?
Common alcohol dependence and withdrawal symptoms include cravings, loss of control, tolerance, and withdrawal reactions such as tremors, insomnia, or nausea when alcohol use is reduced. Behavioral changes like neglecting responsibilities, risky drinking behavior, or continued use despite consequences also point to AUD. The intensity of symptoms often reflects the severity level—mild, moderate, or severe.
4. What Are the DSM-5 Criteria for Alcohol Use Disorder?
The DSM-5 criteria for Alcohol Use Disorder consist of 11 specific symptoms evaluated over a 12-month period. These include drinking more than intended, unsuccessful attempts to cut down, craving, neglecting major obligations, and continued use despite problems. Meeting 2–3 symptoms indicates mild AUD, 4–5 moderate, and 6 or more severe. These criteria are vital in substance use and dependence classification within modern psychiatry.
5. How to Code Alcohol Use Disorder for Clinical Documentation?
Clinicians use ICD-10 mental health codes for accurate diagnostic coding for alcohol-related disorders ****in electronic health records. The primary coding examples for alcohol use disorder include F10.10 and F10.20. Proper clinical documentation for alcohol abuse supports precise treatment planning, continuity of care, and insurance reimbursement.
6. What Are the Key Differences Between Alcohol Abuse and Alcohol Dependence?
Under older diagnostic systems, alcohol abuse referred to harmful drinking behaviors without physical dependence, while alcohol dependence indicated physiological adaptation and withdrawal. The DSM-5 combined these into one diagnosis—Alcohol Use Disorder—with varying severity levels. This shift reflects a more dimensional understanding of substance abuse ICD-10 reference categories used today.
7. What Is the Difference Between F10.10 and F10.20?
The key difference lies in the presence of dependence and severity of symptoms.
F10.10 – Alcohol abuse, uncomplicated: This code represents mild Alcohol Use Disorder without physical dependence, withdrawal, or major complications.
F10.20 – Alcohol dependence, uncomplicated: This code indicates moderate to severe AUD, often involving tolerance, craving, and withdrawal symptoms.
Both codes are part of the mental health billing codes used by clinicians for diagnostic accuracy and insurance claims.
8. What Is the DSM-5-TR Code for Alcohol Use Disorder?
In the DSM-5-TR (Text Revision), the diagnosis remains Alcohol Use Disorder (AUD), with no changes to the core diagnostic criteria. The DSM-5-TR integrates the ICD-10-CM codes to ensure consistency between clinical documentation, insurance billing, and international diagnostic systems.
References:
National Institute on Alcohol Abuse and Alcoholism. (2020). Alcohol Use Disorder: A Comparison Between DSM-IV and DSM-5. https://www.niaaa.nih.gov/publications/brochures-and-fact-sheets/alcohol-use-disorder-comparison-between-dsm
American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). American Psychiatric Publishing.
Why other mental health professionals love Mentalyc

“It takes me less than 5 minutes to complete notes … it’s a huge time saver, a huge stress reliever.”
Licensed Marriage and Family Therapist

“It’s so quick and easy to do notes now … I used to stay late two hours to finish my notes. Now it’s a breeze.”
Licensed Professional Counselor

“A lot of my clients love the functionality where I can send them a summary of what we addressed during the session, and they find it very helpful and enlightening.”
Therapist

“Having Mentalyc take away some of the work from me has allowed me to be more present when I’m in session with clients … it took a lot of pressure off.”
LPC