In 2026, choosing the best AI scribe for therapists is no longer about “saving time.” For therapists, psychiatrists, and medical clinicians, the real question: Can the AI medical scribe tool support clinical reasoning, preserve documentation integrity, and reduce compliance risk – without adding friction to care?
This ranked list of the top 10 best AI therapy scribes in 2026 is written specifically for mental health clinicians. Each tool is evaluated on clinical accuracy, workflow realism, EHR integration depth, privacy safeguards, and compliance readiness based.
Ranked List: Top 10 AI Medical Scribe for Clinicians (2026)
| Rank | AI Medical Scribe | Session Transcription Accuracy | Customization | EHR Integration | Privacy | Security & Compliance | Pricing Range | Overall Rating |
|---|---|---|---|---|---|---|---|---|
| #1 | Mentalyc | Clinical-grade, psychotherapy-specific accuracy with minimal edits required | Highly flexible (SOAP, DAP, BIRP, GIRP, PIRP, custom templates) | Chrome extension mapping directly into EHR fields | Strong: no recordings stored; therapist-controlled | HIPAA + PHI + SOC 2 compliant | $14.99–$99.99 · Free 14-day trial | A+ |
| #2 | Freed AI | Good general clinical accuracy across specialties | Good template adaptability | Browser / EHR push workflows | Standard | HIPAA | Starts at $99 | A |
| #3 | Suki AI | Voice recognition; general clinical accuracy | Moderate template and command control | Deep enterprise EHR integrations (Epic, Athena, etc.) | Standard | HIPAA | Starts at $299 | A |
| #4 | DeepScribe | Solid ambient accuracy; specialty-oriented | Good clinician voice learning | Enterprise EHR integrations | Standard | HIPAA | ~$750/month | A- |
| #5 | Abridge | Contextual summaries | Limited clinician editing control | Enterprise (Epic-focused) | Standard | HIPAA | ~$208/month | B+ |
| #6 | Twofold Health | Good outpatient accuracy | Custom templates available | Browser / EHR push | Standard | HIPAA / BAA | $69/month | B+ |
| #7 | Heidi Health | Transcription with structured drafts | Template control available | EHR via partners | Standard | HIPAA | $99/month | B+ |
| #8 | SimplePractice Note Taker | Adequate therapy drafts; more editing required | Basic customization (SimplePractice only) | Native to SimplePractice | Standard | HIPAA / HITRUST | Included in plans | B |
| #9 | Nabla Copilot | Lightweight assistance; lower clinical depth | Limited templates | Moderate integrations | Standard | HIPAA | Varies / free tiers | B- |
| #10 | Blueprint AI Tools | Documentation support with limited clinical depth | Moderate customization | Selective integrations | Standard | HIPAA | Varies | C+ |
What to Look for in an AI Medical Scribe for Therapists
1. Clinical Accuracy
This is the non-negotiable foundation. A high-quality AI scribe for counseling notes must:
- Correctly interpret medical terminology, psychiatric language, and abbreviations
- Handle negations and risk statements accurately
- Reflect clinical reasoning, not just verbatim transcription
- Generate structured, ready-to-chart notes (SOAP, DAP, etc) that require minimal correction
- Offer transparency or review controls so clinicians can confidently sign notes without second-guessing hallucinations
If accuracy fails here, time savings become liability.
2. EHR Integration & Real-World Workflow Fit
A scribe that lives outside your EHR creates duplicate work. Look for tools that:
- Push notes directly into EHR fields instead of copy-paste
- Preserve structure and formatting inside the EHR
- Support telehealth, in-person, group, and supervision workflows
- Allow clinicians to review, edit, and finalize without breaking focus
True automation means less context-switching, not just faster typing or surface-level real time clinical note generation.
3. Customization That Matches Clinical Style
Documentation isn’t generic—and neither should your AI be. Strong AI scribe for behavioral health:
- Allow template customization across modalities and settings
- Adapt to narrative vs. bullet styles
- Preserve clinician voice rather than rewriting everything into a generic tone
- Support specialty-specific needs (mental health, psychiatry, family therapy, group work)
Customization is about clinical ownership, not aesthetics.
4. Security and Compliance Standards Clinicians Expect from a HIPAA-Compliant AI Scribe
HIPAA compliance alone is not enough in 2026. Evaluate whether the tool:
- Is HIPAA compliant and independently audited (e.g., SOC 2 Type II)
- Uses encrypted processing and secure infrastructure
- Clearly defines data ownership and deletion rights
- Minimizes data retention wherever possible
Compliance should reduce anxiety—not introduce new questions during audits.
5. Privacy-First Design
Especially critical in therapy and behavioral health. Best-in-class tools:
- Do not store session recordings
- Do not use client data to train AI models
- Allow clinicians to delete transcripts, notes, and records at will
- Provide consent-friendly workflows that support ethical practice
Privacy is not a feature—it’s a prerequisite.
6. Choosing an AI Scribe for Clinicians That Fits Your Specialty and Practice Model
Not all tools are built for mental health. Before choosing an AI scribe for private practice therapists or group practices, ask:
- Does the tool understand psychotherapy language and relational context?
- Can it support longitudinal care, not just single visits?
- Does it connect notes to treatment plans and progress over time?
The best AI medical scribe in 2026 supports continuity of care, not isolated documentation tasks.
Mentalyc — #1 Overall Best AI Scribe for Therapists in 2026
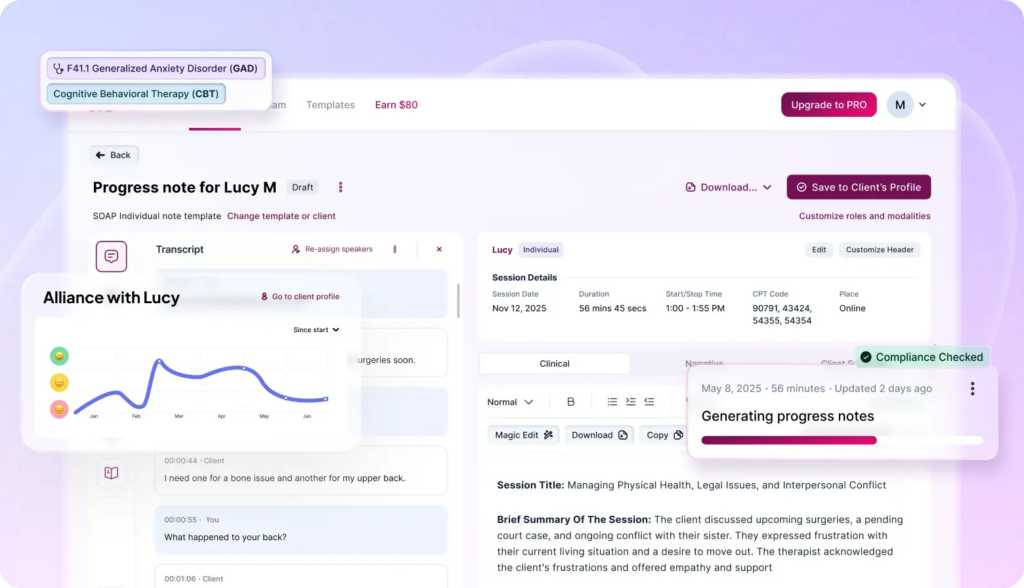
Mentalyc is an AI scribe designed for mental health professionals, focused on saving time by automatically generating insurance ready clinical notes and insights from session audio. It offers significant documentation burden reduction, potentially cutting note-writing time by up to 90%.
Mentalyc provides a user-friendly, secure (HIPAA-compliant) AI assistant that serves as an “unbiased secretary” to create accurate, audit-ready session notes from conversation. The AI generated progress notes allow therapists to be more present with clients and avoid burnout caused by extensive manual documentation.
Key Features

- Write notes without rewriting your day The AI therapy scribe turns session audio, live listening, or dictation into complete, insurance-ready notes (SOAP, DAP, BIRP, GIRP, PIE, and more), so you spend less time editing and more time focused on care.
- Works across therapy types and modalities Whether you see individuals, children, couples, or families- or practice EMDR or Psychiatry; Mentalyc adapts to your clinical context without forcing a one-size-fits-all structure.
- Turn clinical work into clear treatment direction The AI Treatment Planner helps you translate session content into SMART goals, relevant interventions, and ongoing goal tracking – supporting continuity without extra paperwork.
- See the therapeutic relationship more clearly Alliance Genie™ provides supervision-style insights into attunement, collaboration, and rupture-repair patterns, helping you reflect on the alliance without surveys or in-session disruption.
- Built for real clinical privacy standards Mentalyc is fully HIPAA-compliant, designed to protect sensitive client data while keeping clinicians in control of review and interpretation.
- Make sense of complex cases over time Session analytics surface patterns across sessions, such as symptom trends and engagement shifts, supporting stronger case conceptualization without rereading months of notes.
Pros
- One of the most accurate clinical language and highest clinical accuracy in the market
- Fastest workflow – saves hours weekly with true note-taking automation
- Fit different therapy setups, clients, approaches, etc.
- Strongest privacy and security model (HIPAA + PHIPAA + SOC 2 Type II)
- Strengthens clinical insight – helping therapists understand patterns across sessions that inform better care
- Designed to scale as its team plan smoothly into group-practice environments
Cons
- Designed specifically for mental health documentation, so it’s not suited for broader medical use cases.
- No built-in telehealth platform, but works smoothly with whatever tools clinicians already prefer (e.g., Zoom, Doxy).
Best For:
Therapists, counselors, social workers, psychologists, and PMHNPs who want fast, accurate automated therapy documentation.
Works well for solo providers, group practices, supervision teams, and agencies across all therapy formats. Many users consider it as the best AI scribe for group practices.
Pricing:
- FREE Trial (USD 0) — 14 days of full PRO access, including 15 notes; no credit card required.
- Mini (USD 14.99/month billed annually) — For small caseloads. Everything you need to get started.
- Basic (USD 29.99/month billed annually) — For part-time work. Core features to save time and stay flexible.
- Pro (USD 59.99/month billed annually) — For full-time therapy. Powerful tools for deeper insights.
- Super (USD 99.99/month billed annually) — For unlimited use. All features unlocked. no limits, full control.
Visit the pricing page for more details.
Freed AI — Practical Documentation Assistant
Freed AI is positioned as a lightweight AI medical scribe for clinicians who want fast documentation without workflow complexity. Its core strength is simplicity: setup is minimal, the interface is straightforward, and note generation works well for routine, low-complexity visits.
However, this simplicity also limits flexibility. Template options and customization controls are relatively narrow, which can make the tool feel restrictive for clinicians managing nuanced presentations or layered clinical reasoning. One clinician review captures this trade-off clearly:
“…but it felt like there wasn’t much flexibility, just a few templates and not much ability to tweak how it works. Output was good for simple visits, but not robust enough for my more complex cases.” — Freed AI user, via Reddit
Key Features
- Listens and transcribes patient encounters (in-person or virtual).
- SOAP Note Generation: Creates structured notes (Subjective, Objective, Assessment, Plan) with patient instructions.
- Customization: Supports custom templates and learns from clinician edits.
- Multi-Language Support: Works in over 14 languages.
- EHR Compatible: Allows copy-pasting into any EHR system.
- Magic Edit: In-app editing for quick adjustments.
Pros
- Saves Time: Reduces documentation burden, freeing up clinician time.
- Accuracy & Speed: Fast, accurate transcription, often requiring minimal editing.
- Ease of Use: Simple interface, low learning curve.
- Specialty-Specific: Customizable for different medical fields.
- HIPAA Compliant AI Scribe: Secure for patient data.
Cons
- Cost: Can be expensive for large practices.
- Limited EHR Integration
- Noise Sensitivity: Performance can suffer in very noisy environments.
- Occasional Misinterpretation: AI may misinterpret complex conversations.
Best For
- Solo practitioners or small groups focused on ease of use and quick setup.
- Clinicians wanting to reclaim time from documentation.
- Providers needing support across multiple languages.
Pricing
- Individual (Monthly): ~$99/user.
- Individual (Annual): ~$90/user/month (paid upfront).
- Small Group (2-9): ~$84/user/month (annual contract).
- Large Group (10+): Custom Quote.
Suki AI — Voice-First Medical Scribe with EHR-Centric Workflows
Suki AI is positioned as a voice-first AI medical assistant designed to support real-time dictation and documentation across medical specialties, with deeper adoption in physician-led workflows. When functioning well, it can streamline note creation through voice commands and EHR-connected dictation.
However, clinician feedback suggests that reliability and consistency have been concerns in recent iterations. Workflow disruptions, unexpected text behavior, and declining dictation accuracy can undermine clinical efficiency—particularly during live documentation. One clinician review reflects this experience:
“For the past several months the program became glitchy. It would suddenly start erasing and reinserting dictated text, include prior notes at the cursor location, and freeze my cursor for 30–60 seconds…” — Suki AI user via Capterra.
Key Features
- Listens to patient-doctor conversations to generate full clinical notes, patient instructions, and orders.
- Voice-Enabled Commands: Allows clinicians to use voice for editing, navigating the EHR, and adding information.
- Customizable Notes: Adapts to different workflows with problem-based charting and tailored drafts.
- Order Staging: Helps review and sign orders directly from the encounter.
- EHR Integration: Syncs notes directly to the Electronic Health Record.
- Billing & Coding: Can generate billing codes and other data.
Pros
- Automates documentation.
- Good for voice commands and EHR interaction.
- Captures more than just transcription, creating complete notes.
- Supports Many Languages: Handles over 80 languages.
Cons
- Cost: Can be expensive, targeting larger organizations.
- Complexity: May involve a more complex setup than simpler alternatives.
Best For
- Large Health Systems: Ideal for hospitals and large groups with established IT and a need for deep workflow automation.
- Clinicians Needing Strong Voice Control: Best for those who prefer dictating and navigating via voice.
Pricing (Estimated)
Enterprise-Focused: Pricing is often quoted in the range of $350-$500+ per provider per month, with some sources citing around $399/month, targeting larger clients.
DeepScribe — Ambient Scribing, Infrastructure Dependency Risks
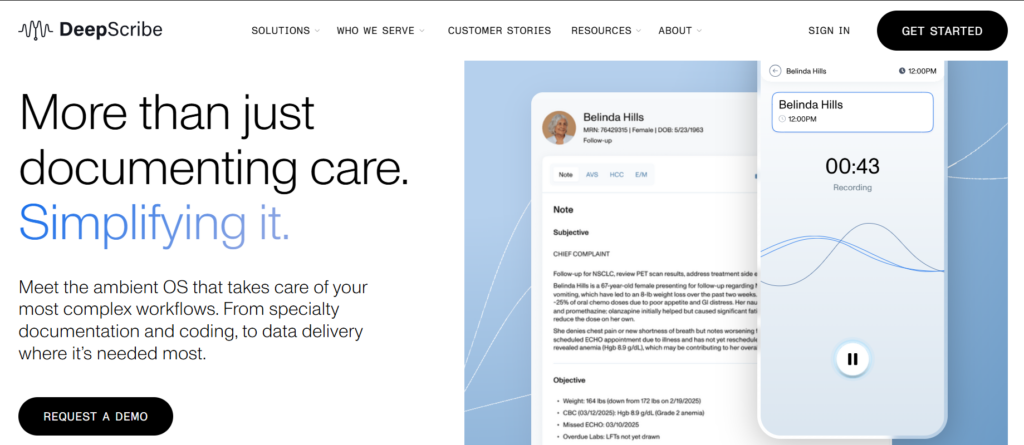
DeepScribe is positioned as an ambient AI scribe designed to passively capture and document clinical encounters, particularly in busy outpatient and physician-led settings. When functioning as intended, it can reduce active documentation effort by generating detailed transcription-based notes.
However, clinicians have raised concerns about system reliability and infrastructure dependency, especially when availability issues disrupt access to same-day documentation. One clinician experience highlights this operational risk:
“I rely on DeepScribe AI transcription notes and DeepScribe relies on Amazon Servers, which goes down from time to time without advance notice and sometimes all of my transcriptions for the day are lost!…” — DeepScribe user Via G2.
For practices that depend on consistent uptime and guaranteed access to session data, this reliance on third-party infrastructure may introduce workflow risk and necessitate backup documentation processes.
Key Features
- Listens to conversations in real-time, capturing details without disrupting patient interaction.
- Works with major EHRs (Epic, Cerner, etc.) to auto-populate notes.
- Offers tailored AI for oncology, primary care, cardiology, and more, with customized templates.
- Provides diagnosis suggestions, HCC code insights, and auto-orders.
- Multilingual Support: Handles patient conversations in over 25 languages.
Pros
- Reduction in documentation time (up to 75% reported).
- Improved accuracy with deep learning and human review options.
- Enhances patient care by allowing focus on the patient.
- Strong market leader with high user satisfaction for ease of use and quality.
Cons
- Pricing is hidden: Requires a demo and call for costs, can be expensive for small practices.
- Editing still required: Notes need clinician review and modification.
- Setup & Training: Can be complex and time-consuming.
- Mobile Limitations: Some users report issues with app stability on phones.
- Limited EHR Integration: Some users report less direct integration than competitors, often requiring copy-paste.
Best For
- Busy specialty practices, especially oncology, looking for deep EHR integration and customizable workflows.
- Clinicians aiming to reduce burnout and improve efficiency.
- Clinics that need multilingual support for diverse patient populations.
Pricing
Not publicly listed: Requires a demo and custom quote; costs vary but are considered high for small groups. Older sources suggest around $750/month as a potential range for some users, but this isn’t official.
Abridge — Smooth Summaries, Limited Clinical Reasoning Capture
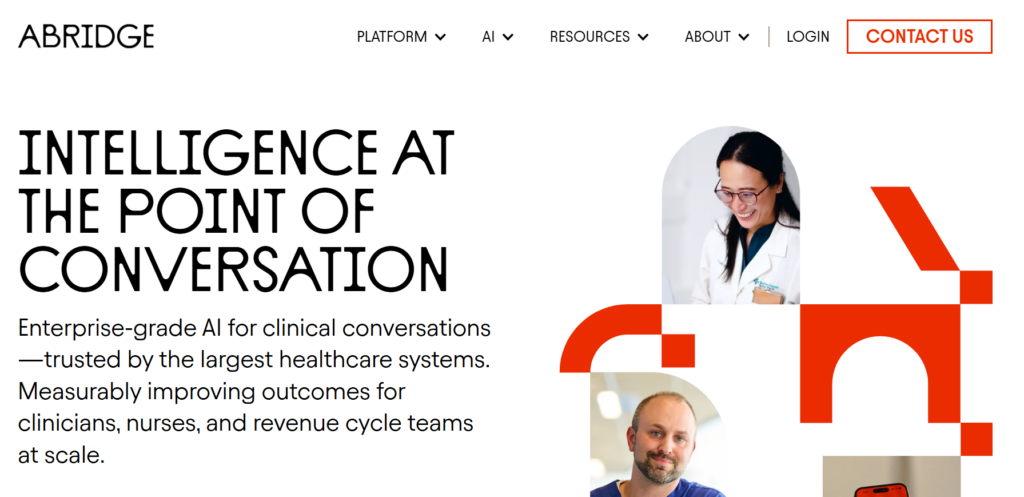
Abridge is designed as a conversation-focused clinical AI that emphasizes generating clear, readable summaries from patient–clinician interactions. It performs smoothly in capturing and organizing dialogue, making it useful for high-level encounter documentation and patient-facing summaries.
However, clinicians have noted that while the surface-level documentation is polished, the tool can occasionally miss the clinical reasoning and decision-making that underpins assessment and treatment plans. One clinician review captures this limitation succinctly:
“Abridge was smooth but sometimes missed the reasoning behind my plan.” — Abridge user via Reddit.
For clinicians whose documentation relies heavily on explicit medical necessity and clinical judgment, this gap may require additional manual clarification before finalizing notes.
Key Features
- Listens to conversations and generates drafts of clinical notes.
- Integration with systems like Epic and Meditech.
- Uses large language models for summarization and formatting.
- Multilingual Support: Handles dozens of languages.
- Configurable templates and formatting for organizational needs.
- Can draft letters, reports, and treatment plans.
Pros
- Decreases after-hours work and cognitive load.
- Saves clinicians time on documentation.
- Supports broad medical specialties.
Cons
- Cost: Can be more expensive than budget options, with enterprise pricing potentially high.
- Deployment: IT-heavy deployment for large systems.
- Limited Free Access: Enterprise models often lack free trials.
Best For
- Large Healthcare Systems: Especially those using Epic or Meditech, due to deep integration.
- Clinicians Seeking Efficiency: Providers wanting to reduce documentation burden and burnout.
- Multilingual Practices: Where language barriers are a concern.
Pricing
Enterprise Focus: Pricing is typically enterprise-level, not listed for individual users.
Twofold Health — Minimalist AI Scribing for Routine Documentation
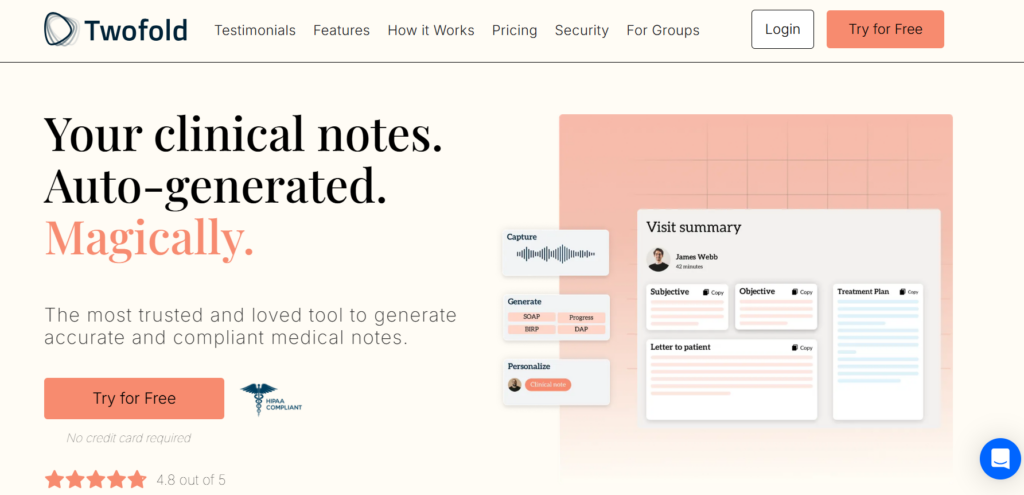
Twofold Health is a lightweight AI medical scribe focused on speed and ease of use rather than advanced clinical intelligence. It is designed to help clinicians quickly generate structured note drafts for routine outpatient visits, with minimal setup and a simple capture workflow. Customization and specialty-specific depth are limited, and EHR workflows typically rely on manual transfer rather than direct field-level integration. From a compliance perspective, it follows standard HIPAA requirements, but it is best suited for clinicians who want a straightforward documentation assist rather than a deeply integrated or clinically nuanced scribing system.
Key Features
- Creates full SOAP/progress notes from patient encounters, often in under a minute.
- Accepts direct audio, uploaded summaries, or manual summaries for note creation.
- Allows easy copy-paste or integration into existing EHR/EMR systems.
- Learns clinician’s style and improves over time.
Pros
- Minimal setup, ideal for small practices.
- Competitive pricing compared to human scribes.
- Versatile Input: Adapts to different practice workflows (live audio, summaries).
- Accessibility: Mobile and desktop apps for flexibility.
Cons
- Review Needed: Output may require significant editing for complex cases or poor templates.
- Potential Errors: Can miss or misrepresent clinical details, requiring thorough review.
Best For
- Solo practitioners and small clinics.
- Clinicians in primary care, behavioral health, and therapy.
- Providers seeking an affordable, easy-to-implement solution.
Pricing (Approximate)
- Free Tier: Basic note creation available.
- Personal Plan: ~$49-$69/month (billed annually/monthly) for unlimited notes.
- Group/Enterprise: Custom pricing with volume discounts and organizational support.
Heidi Health — Structured Notes, Limited Clinical Depth
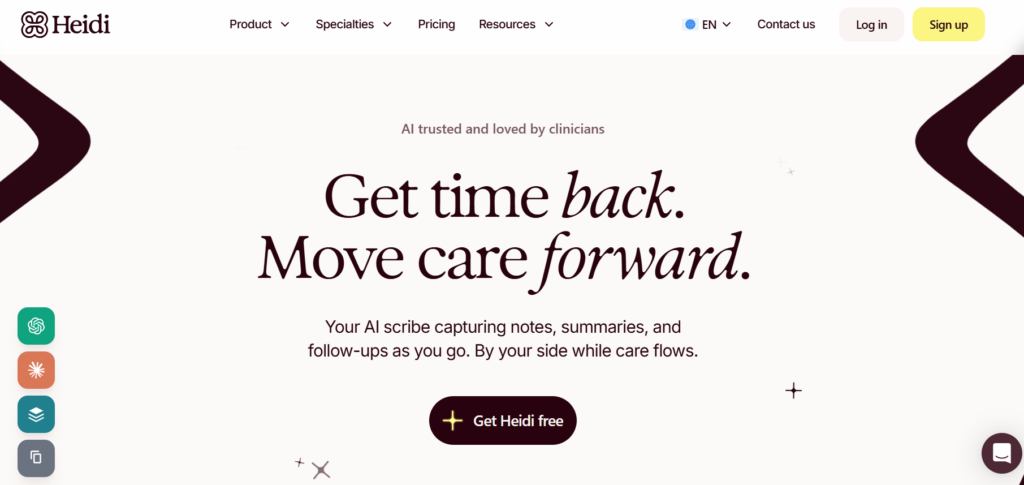
Heidi Health positions itself as an AI scribe focused on producing structured clinical notes with optional customization through paid plans. It performs reliably for standard documentation workflows and appeals to clinicians who want predictable output aligned with their own templates.
That said, its scope remains narrowly focused on note generation. Clinical decision support and medical Q&A are intentionally limited, and feature development appears incremental rather than rapid. A clinician review reflects this balance between stability and constraint:
“…Their chat functionality doesn’t answer medical questions, which I think a medical scribe should be able to do. They also seem really slow to add new features—their public roadmap has had ‘coming soon’ items sitting there forever.” — Heidi Health user via Reddit.
Key Features
- Real-time Documentation
- Accessible on web, desktop, and mobile devices.
- Offers template customization and a community template library.
- Generates referral letters, patient summaries, and follow-up tasks.
- Connects with electronic health records for seamless workflow.
Pros
- Time Savings: Reduces documentation burden, returning hours to clinicians.
- Cost-Effective: Offers a free plan and affordable Pro pricing.
- Flexibility: Adapts to different specialties and workflows.
- Workflow Support: Helps with coding suggestions and task management.
Cons
- Audio Dependency: Performance relies on clear audio from recordings.
- Feature Gating: Advanced features are reserved for paid tiers.
- Potential for Disruption: Like any new tool, requires adaptation to workflow.
Best For
- All Specialties: Used across over 200 medical specialties, from general practice to specialized fields.
- Clinicians Seeking Efficiency: Ideal for providers wanting to reduce administrative work and focus on patient care.
Pricing (Approximate)
- Free: Unlimited standard transcription, basic templates, healthcare security.
- Pro: Around $90-$100/month (annual billing), adding advanced templates, “Ask Heidi,” and more.
- Practice: Around $120/month (annual), including session sharing, free assistant users, priority support.
- Enterprise: Custom pricing for large organizations
SimplePractice Note Taker — Convenience Inside the EHR, Privacy Concerns
SimplePractice offers an AI note-taking feature embedded within its EHR, positioned as an add-on for clinicians who already document inside the platform. While this tight integration can reduce workflow friction for providers, client feedback highlights concerns around usability limitations and perceived privacy transparency, particularly from the client perspective. One client review reflects these concerns clearly:
“I am a CLIENT of a psychotherapist who uses this. It only works on phones and iPads–not laptops, so the visual is small and unsatisfactory. The terms of service provide NO ASSURANCE of privacy, and the Bot-driven help makes me think…” — Teri Bernstein, via Trustpilot
For clinicians, this underscores an important consideration: documentation tools can affect client trust, especially when usability constraints or unclear privacy messaging surface during sessions.
Key Features
- Generates session notes (SOAP, DAP, BIRP) from audio recordings or dictation.
- Adapts to your clinical style with edits, keeping notes authentic.
- HIPAA Compliant
- Connects with SimplePractice’s practice management features.
Pros
- Saves Time: Reduces time spent on post-session documentation.
- Focus on Clients: Allows therapists to focus on the session, not typing.
- Secure: HIPAA-compliant with advanced security protocols.
- Versatile: Works with live recording, dictation, or uploaded audio/text.
Cons
- Requires Review: AI drafts need editing to fully match your voice and ensure accuracy.
- Add-On Cost: Not included in base plans; costs extra.
- Learning Curve: May need training for optimal use, like any new tool.
Best For
- Solo therapists and group practices focused on efficiency.
- Clinicians who value HIPAA-compliant, automated note generation.
- Practices looking to enhance client engagement by reducing admin time.
Pricing
- Core Plans (SimplePractice): Starter ($29/mo), Essential ($69/mo), Plus ($99/mo).
- Note Taker (Add-On): Approximately $35/month (after a free trial).
Nabla Copilot — Lightweight Scribe With Limited Depth
Nabla Copilot is positioned as a lightweight AI scribe with an emphasis on simplicity and ease of use. Its clean interface and minimal setup make it approachable for clinicians who want quick documentation support without complexity.
However, that same minimalism limits depth. Customization options and specialty-specific controls are relatively sparse, which can affect accuracy and usefulness for more complex or nuanced clinical encounters. A clinician review summarizes this trade-off:
“…If you want something super simple, it’ll do the trick, but most of us need more control and accuracy. Lacks a lot of specialty/custom options.” — Nabla user via Reddit.
Key Features
- Converts natural conversation into structured notes (SOAP, progress notes).
- Listens in the background during in-person, video, or phone consultations without disrupting the flow.
- EHR Integration
- Multi-language Support
- Cross-Platform Accessibility: Available via web app, mobile app, and a Chrome extension.
Pros
- Time Savings
- Standard Clinical Accuracy
- Emphasizes privacy with a design that avoids storing patient data on external servers.
Cons
- Narrow Focus: Primarily built only for clinical documentation, which may create information silos if an organization needs AI solutions for other departments (e.g., IT, patient support).
- Reliance on Copy-Paste: For some EHR systems, integration relies on a copy-paste workflow or browser extension rather than a direct API connection.
- Potential for Errors: It can struggle with very complex cases, diverse accents, or background noise, and can occasionally “hallucinate” or generate slightly incorrect information, requiring clinician review.
Best For
This tool is ideal for individual clinicians and small practices seeking an efficient, affordable solution to the daily pain of documentation. The Enterprise plan is suitable for hospitals, large clinics, and telehealth companies needing custom integrations, advanced security, and dedicated support.
Pricing
- Free Plan: Suitable for interns, residents, or testing, with limits on monthly consultations.
- Pro Plan: $119/month per clinician for unlimited notes and EHR integration.
- Enterprise: Custom pricing for larger entities requiring advanced security and integrations.
Blueprint AI — Simple AI Therapy Scribe for Clinical Notes
Blueprint is positioned as a mental health–focused documentation tool with an emphasis on structured notes and technique-driven summaries. While the platform aims to support clinical workflows, clinician feedback suggests variability in note quality. Notes may overemphasize lists of techniques while underrepresenting clinically meaningful content, and assessment sections can feel repetitive rather than interpretive. As a result, clinicians may spend significant time revising drafts to restore clarity and accuracy. One clinician review describes this experience:
“Often notes are not accurate—they list techniques so that is the majority of the note. The assessment section is literally just repeating what was already said, which feels like a waste. Often key content is lost or non-existent…” — Apricot Cream Meadowlark, via Blueprint Feedback Portal
For clinicians who value concise assessments and reliable capture of core clinical content, this level of inconsistency may reduce the tool’s overall time-saving benefit.
Key Features
- AI-Powered Documentation
- Workflow Flexibility
- Customization
- Golden Thread Tracking
- HIPAA-compliant with robust encryption, advanced privacy controls, and signed Business Associate Agreements (BAAs).
Pros
- Designed for mental health workflows, addressing the need for specialized documentation and insights.
- Reduces time spent on administrative tasks, allowing clinicians to focus on patient care and potentially see more patients.
- The AI generates structured and standardized notes, which can lead to better clarity and potentially fewer claim denials.
- Eliminates the distraction of typing during sessions, leading to more engaged and personal patient interactions.
Cons
- Niche Focus: Features might be less relevant or suitable for medical specialties outside of mental/behavioral health compared to general AI scribes.
- Customization Efforts: While highly customizable, the initial setup to fine-tune preferences and templates might require some upfront effort.
- Potential Unpredictability: In a usage-based model, costs can be unpredictable for busy periods, which might exceed a flat-rate subscription cost.
Best For
Blueprint AI is best for:
- Mental and behavioral health clinicians (individual, couples, or group practices) seeking a specialized AI solution.
- Practices that value data analytics and risk assessment metrics integrated with their documentation.
- Clinicians who want a highly customizable AI that learns their specific note-taking style over time.
Pricing
Blueprint offers modular, session-based pricing plans:
- Standard: $0.49 per session for AI-assisted documentation.
- Plus: $0.99 per session for documentation and clinical support features.
- Pro: $1.49 per session (coming soon) with advanced features and EHR integration.
- A free trial is available, and enterprise/volume pricing is also offered.
Final Recommendation: Which is the Best AI Scribe in 2026 for Therapists?
Choosing the best AI scribe for therapists in 2026 depends less on feature count and more on clinical fit, reliability, and documentation integrity. Many tools on the market perform well for basic transcription or simple visit summaries, but begin to show limitations when cases become complex, workflows span multiple sessions, or documentation must clearly demonstrate medical necessity.
For clinicians who want simple draft notes for routine visits, lightweight tools like Freed AI, Nabla, or Twofold Health can reduce initial typing time—but they often require consistent editing and manual EHR transfer. Enterprise-focused solutions like DeepScribe, Suki AI, and Abridge offer broader infrastructure and ambient capture, yet may introduce trade-offs around reliability, clinical reasoning depth, or privacy preferences.
For mental health clinicians in particular, Mentalyc stands out for supporting the entire documentation workflow: clinically accurate notes, customizable templates, treatment planning, progress tracking, and privacy-first design—all while keeping the clinician fully in control. Rather than optimizing only for speed, it prioritizes accuracy, continuity, and audit-ready documentation, which ultimately determines whether an AI scribe truly saves time or creates downstream work.
FAQs: Best AI Scribe for Therapists in 2026
1. Are AI medical scribes accurate enough for clinical documentation?
AI medical scribes can significantly reduce documentation time and support clinical documentation automation, but they are not autonomous clinicians. Accuracy varies by tool, case complexity, and audio quality. All AI-generated notes should be reviewed and signed by the clinician, especially for assessments, risk statements, and treatment plans.
2. Can AI medical scribes replace manual note-writing entirely?
No. AI scribes generate drafts, not final clinical judgments. The best tools reduce repetitive typing and structure notes intelligently, but clinicians remain responsible for clinical reasoning, accuracy, and compliance.
3. How important is EHR integration when choosing an AI scribe for Therapists?
Very important. Tools that require repeated copy-paste or reformatting can negate time savings. Deeper EHR integration—especially field-level insertion—reduces friction and documentation fatigue over time.
4. Are AI medical scribes safe and HIPAA-compliant?
Most reputable tools are HIPAA-compliant, but clinicians should look beyond labels. Important factors include whether recordings are stored, whether data is used to train AI models, encryption standards, and whether the vendor undergoes independent security audits (e.g., SOC 2).
5. Which AI medical scribe is best for mental health clinicians?
Mental health documentation requires nuance, longitudinal continuity, and strong privacy safeguards. Tools like Mentalyc are specifically designed as an AI scribe for psychotherapy—rather than general medicine. They tend to perform better for psychotherapy, psychiatry, group sessions, and treatment planning.
Why other mental health professionals love Mentalyc

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“Do yourself a favor, make your life easier. I found Mentalyc to be one of the best tools that I’ve ever used.”
Licensed Marriage and Family Therapist

“For anyone hesitant: this is a lifesaver. It will change your life, and you have more time to be present with your patients.”
Licensed Clinical Social Worker

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)