Intake notes form the foundation of a treatment plan. They capture a client’s history, current concerns, and initial goals during the early sessions—including presenting problems, mental and medical history, family background, risk factors, and functional impairment. A treatment plan translates that information into a clear clinical roadmap by defining the diagnosis, treatment goals, objectives, and planned interventions that will guide care moving forward.
For many clinicians, this transition is where documentation breaks down. Intake notes are rich but sprawling. Treatment plans feel forced, generic, or disconnected from what actually happened in session. And when plans don’t clearly reflect the intake, the “golden thread” of care is lost—creating risk during audits, utilization reviews, or clinical handoffs.
This guide walks through how to turn intake notes into a treatment plan using sound clinical reasoning, diagnosis-driven logic, and documentation best practices—while showing how tools like Mentalyc can support the process without replacing clinical judgment.
Why the Intake to Treatment Plan Transition Matters
| Intake Notes | Treatment Plan |
|---|---|
| Captures raw information | Synthesizes meaning |
| Broad and exploratory | Focused and selective |
| Past- and present-oriented | Future-oriented |
| Descriptive | Justificatory and strategic |
The shift from intake notes to a treatment plan is one of the most consequential moments in therapy documentation. It’s where clinical understanding becomes clinical direction and where documentation either holds together under scrutiny or begins to unravel. A well-executed transition does more than satisfy paperwork requirements; it shapes how care is delivered, evaluated, and defended over time.
Intake notes are descriptive; treatment plans are directive
Intake notes are designed to capture information. They document the client’s story, symptoms, history, and initial impressions—often in the client’s own words. This information is intentionally broad because its purpose is assessment. A treatment plan, by contrast, is decisional. It answers a different set of questions:
- What problems are we prioritizing?
- Why is treatment clinically necessary?
- What changes are we aiming for, and how will we pursue them?
The transition matters because it requires synthesis. Not every detail from the intake belongs in the plan. The clinician must decide what is clinically central, what is contextual, and what will guide treatment moving forward.
Demonstrates medical necessity
From a compliance standpoint, the treatment plan is where medical necessity becomes explicit. Reviewers are not evaluating whether the intake was thorough. They are evaluating whether the information gathered justifies ongoing care. A defensible plan clearly connects:
- Symptoms and functional impairments identified at intake
- A diagnosis that explains those impairments
- Goals and interventions that logically address them
When this connection is missing or vague, documentation risk increases; regardless of how clinically sound the therapy itself may be.
Translates assessment data into intentional care
Assessment data alone does not demonstrate clinical reasoning. Treatment planning does. This step shows how the clinician moved from “what is happening” to “what we are going to do about it.” It explains why certain problems were prioritized, why specific goals were chosen, and why particular interventions make sense given the diagnosis and client context.
Well-written plans signal intentional, diagnosis-driven care, rather than generic therapy that could apply to anyone.
Establishes a forward-looking clinical roadmap
A treatment plan is not a summary of the intake, it is a map for future work. For clinicians, this provides structure and continuity. For clients, it clarifies purpose and expectations. For reviewers, it demonstrates that treatment is planned, monitored, and revisited; not improvised session by session. It outlines:
- The direction of treatment
- What meaningful progress should look like
- How change will be evaluated over time
Maintains alignment with progress notes over time
The treatment plan serves as an anchor for future progress notes. When goals and objectives are clearly defined, each session can be documented in relation to them—preserving the “golden thread” across care. This alignment makes it easier to:
- Justify interventions used in session
- Show how sessions build toward goals
- Update plans meaningfully as treatment evolves
Without this anchor, progress notes often drift into isolated narratives that are difficult to defend collectively.
Meets the expectations of reviewers and collaborators
Payers, supervisors, and future clinicians are not looking for every detail from the intake. They want clear evidence that:
- You accurately understood and prioritized the assessment data
- You formulated a clinically appropriate diagnosis
- You designed a treatment plan that logically and defensibly addresses the client’s needs
This is where intake assessment synthesis and clinical formulation become essential—bridging information gathered at intake with a coherent, defensible plan for treatment.
Core Components of the Treatment Plan
| Treatment Plan Component | What It Includes | Why It Matters Clinically |
|---|---|---|
| Demographic & Administrative Information | Client identifiers (name, DOB, contact details), insurance information, provider name, session date, and service location | Establishes the legal and administrative context of care and ensures documentation meets billing and compliance requirements |
| Presenting Problems / Chief Complaint | Concise summary of current symptoms, stressors, and the client’s reason for seeking therapy, ideally using the client’s own words | Clarifies the focus of treatment and anchors the plan in the client’s lived experience |
| Biopsychosocial Assessment Summary | Key intake findings such as medical and mental health history, substance use, family and social context, trauma history, and prior treatment experiences | Provides clinical context and informs diagnosis-driven treatment planning |
| Mental Status Exam (MSE) & Risk Assessment | Observations of appearance, mood, affect, behavior, cognition, insight, judgment, and assessment of risk to self or others | Demonstrates ongoing clinical monitoring and supports safety and medical necessity |
| Diagnosis & Medical Necessity | Primary diagnosis (e.g., DSM-5-based) with a clear rationale linking symptoms and functional impairment to the need for treatment | Justifies why therapy is required and supports insurance and audit reviews |
| Goals & Objectives | Broad, client-centered treatment goals paired with SMART, measurable short-term objectives | Translates assessment data into clear targets for change and progress evaluation |
| Interventions | Specific therapeutic approaches and techniques (e.g., CBT, EMDR, mindfulness) along with session frequency and expected duration | Shows how the clinician intends to help the client achieve each goal |
| Anticipated Time Frame & Next Steps | Estimated timeline for goal attainment, review points, follow-up plans, referrals, or additional assessments | Reinforces that the treatment plan is forward-looking and responsive to client progress |
Step-by-Step Guide: Turn Intake Notes into a Treatment Plan
1. Review the Intake Note — Gather Client Information and Diagnosis
Begin by carefully reviewing the intake notes to extract all clinically relevant information. This includes demographic and administrative details, the client’s presenting concerns (ideally in their own words), psychosocial and medical history, identified risk factors, and the initial or provisional diagnosis (for example, DSM-5-TR or ICD-10). This step ensures the treatment plan is grounded in documented assessment data and clearly supports medical necessity.
2. Identify Key Problems and Develop a Focused Problem List
Next, distill the intake information into a concise list of the client’s primary problems and symptom areas that require therapeutic attention. These problems should come directly from the presenting concerns and assessment findings, prioritizing issues that are most impairing, clinically relevant, and appropriate for treatment at this stage.
3. Set Client-Centered Treatment Goals
For each identified problem, collaborate with the client to define broad, long-term goals. These goals should reflect what meaningful change looks like for the client, align with their values and strengths, and remain clearly tied to the presenting issues identified at intake.
Example goal: Reduce anxiety symptoms to improve daily functioning.
4. Break Goals into SMART Objectives
Translate each long-term goal into specific, measurable, achievable, relevant, and time-bound (SMART) objectives. Objectives clarify how progress will be evaluated and provide concrete markers of change over time.
Example objective: Client will practice deep breathing exercises three times daily and record anxiety levels in a journal for the next four weeks.
5. Select Appropriate Clinical Interventions
Identify and document the therapeutic approaches and strategies you will use to help the client meet each objective. Interventions should be evidence-informed, appropriate to the diagnosis, and clearly connected to both the goals and objectives.
Example intervention: Clinician will use Cognitive Behavioral Therapy (CBT) techniques to identify and challenge cognitive distortions related to anxiety triggers.
6. Establish Progress Measures and Session Frequency
Specify how progress toward objectives will be monitored and documented, along with the planned frequency and duration of sessions. This provides structure and reinforces that the plan is time-limited and subject to review.
Example: Sessions will occur weekly for 6–8 weeks, followed by reassessment of goals and progress.
7. Review, Sign, and Revisit the Plan
Finally, review the completed treatment plan with the client to ensure shared understanding and agreement. Obtain required signatures as appropriate. The treatment plan should be treated as a living document—revisited, updated, and refined as the client’s needs evolve and progress is made.
Common Pitfalls When Creating Treatment Plans from Intake (and How Technology Can Help)
Even experienced clinicians struggle with treatment planning—not because of a lack of clinical skill, but because the process is cognitively demanding and time-intensive. When intake notes are dense and time is limited, several predictable pitfalls tend to appear.
Common challenges include:
Copy-pasting intake language without synthesis
Intake notes are exploratory by design. When their language is copied directly into the treatment plan, the result is documentation that describes problems but doesn’t explain how treatment will address them. This weakens clinical clarity and medical necessity.
Writing goals that describe interventions rather than outcomes
Goals like “use CBT techniques” or “process trauma” reflect therapist actions, not client change. This makes it difficult to demonstrate progress or justify continued care.
Overloading the plan with too many goals
Intakes often uncover multiple concerns. When every issue becomes a goal, plans lose focus, become unmeasurable, and are harder to revisit or defend during reviews.
Ignoring risk or medical necessity language
Risk factors, functional impairment, and diagnostic rationale may be documented in the intake but never carried forward into the treatment plan—creating gaps that are red flags for audits and utilization review.
Creating plans that never get revisited
Static treatment plans quickly fall out of sync with real clinical work. When goals aren’t updated as clients progress, documentation loses its “golden thread.”
Importantly, these issues don’t reflect poor clinical care—they reflect workflow strain. Translating rich assessment data into a structured, evolving treatment plan requires time, attention, and cognitive bandwidth that many clinicians simply don’t have between sessions. This is where technology can play a supportive role. Many modern AI-powered documentation tools like Mentalyc help reduce this friction by:
- Pulling relevant data directly from intake notes into treatment plan templates
- Offering structured goal and objective suggestions
- Prompting inclusion of diagnosis, risk, and medical-necessity language
- Making plans easier to update over time
It also helps ensure that treatment plans remain clinically meaningful, measurable, and continuously aligned with intake findings and ongoing session work.
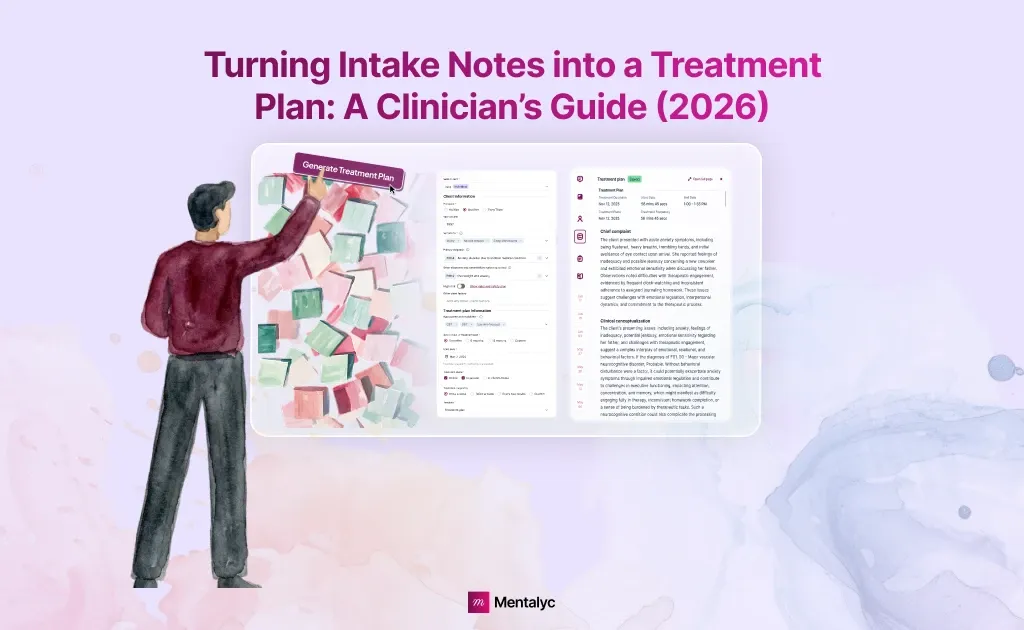
How Mentalyc Supports Turning Intake Notes into a Treatment Plan
Turning intake notes into a treatment plan requires more than speed—it requires clinical coherence. The plan must reflect the assessment, support the diagnosis, guide care forward, and stay aligned as therapy evolves. This is exactly where Mentalyc is designed to help.
Mentalyc doesn’t ask clinicians to start over or work from rigid templates. Instead, it works directly from your intake notes and session recordings, helping your existing clinical documentation become a structured, actionable treatment plan.
From Intake Data to Actionable Care: Automatically, but still Clinically Grounded
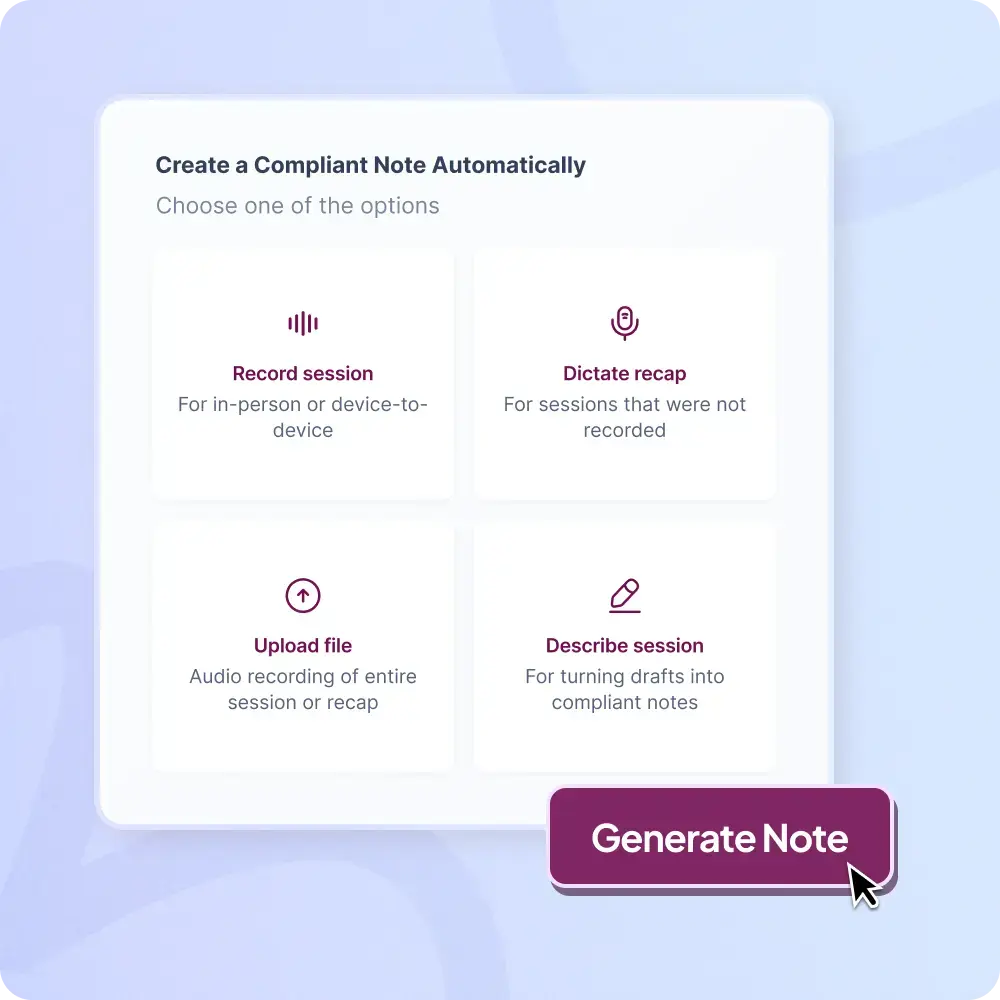
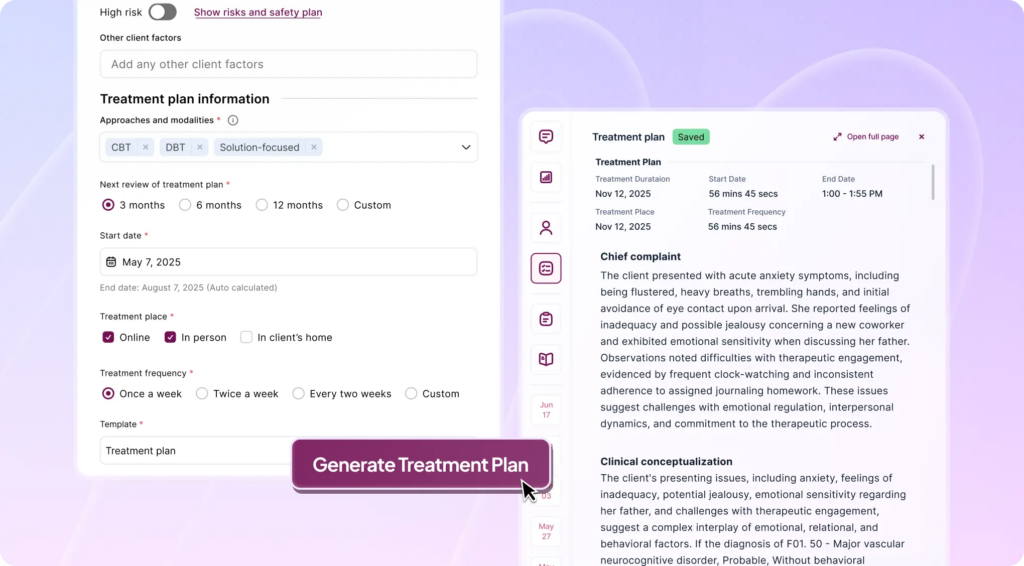
Mentalyc works directly from your intake notes and session recordings, extracting clinically relevant information such as presenting problems, symptom patterns, functional impairment, and diagnostic indicators. From this data, Mentalyc can automatically generate a treatment plan that reflects what was actually assessed—eliminating the need to recreate plans from scratch.
With a single click, clinicians can create an insurance-ready treatment plan, written in clear, structured language that supports medical necessity and audit expectations.
SMART Goals and Interventions – Grounded in Your Notes
One of the most difficult parts of treatment planning is translating broad assessment findings into measurable goals. Mentalyc supports this by suggesting SMART goals and aligned interventions based on the intake content. These suggestions are designed to be:
- Specific and measurable
- Clinically appropriate for the identified concerns
- Directly tied to documented symptoms and diagnosis
Importantly, these are starting points, not final decisions—clinicians remain fully in control.
Preserving the Golden Thread Across Documentation
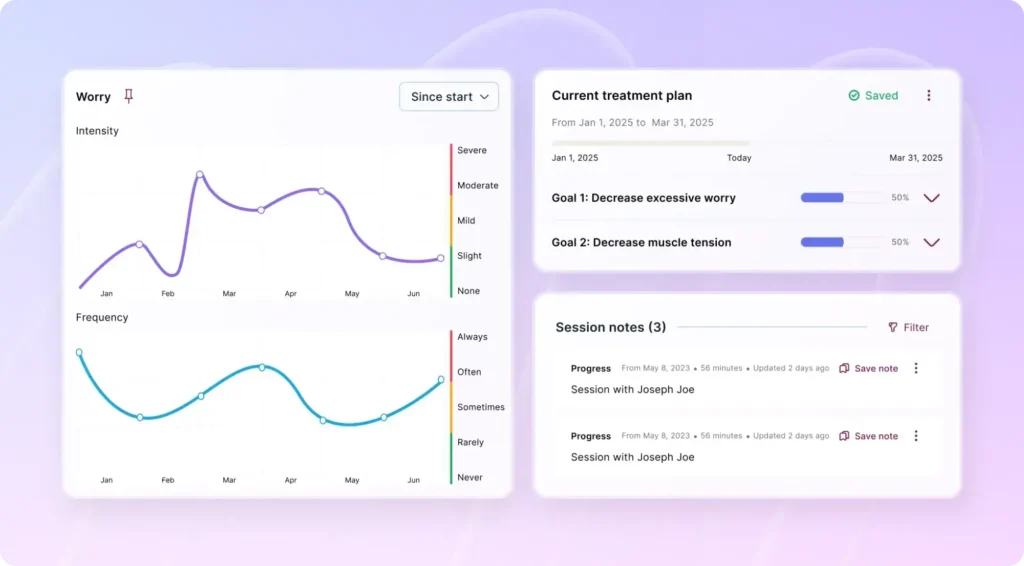
A common documentation breakdown occurs when treatment plans drift away from intake findings or progress notes. Mentalyc maintains alignment by keeping intake notes, treatment goals, and progress notes connected in one continuous story of care. As new sessions are added, the treatment plan remains anchored to the same clinical rationale, preserving the “Golden Thread” that payers and supervisors expect to see.
Treatment Plans That Evolve With Your Client
Mentalyc is designed so treatment plans don’t become outdated the moment they’re written. As new session notes are documented, the plan stays aligned with the client’s current presentation. When symptoms shift, goals can be refined, and progress is recorded, those changes are reflected in the treatment plan – without needing to rewrite it from scratch.
This keeps the treatment plan clinically current over time. Instead of revisiting a static document every few months, therapists can rely on a plan that evolves alongside ongoing session work, preserving continuity of care and reducing documentation overhead.
Customization Without Losing Structure
While Mentalyc can generate treatment plans automatically, it is built to respect clinical individuality. Clinicians can:
- Edit goals and objectives
- Adjust wording to match your therapeutic voice
- Tailor interventions to modality and client needs
This balance ensures efficiency without sacrificing professional judgment or clinical nuance.
Secure, Compliant, and Clinician-Controlled
Mentalyc is fully HIPAA-compliant, using anonymization and encryption to protect client data. Session recordings are not stored, and data is never used for model training. This allows clinicians to leverage AI support with confidence that privacy, ethics, and compliance are fully addressed.
Conclusion: Turning Therapy Intake Documentation into A Treatment Plan
Turning intake notes into a treatment plan is not just paperwork. It’s the moment where clinical understanding turns into a clear plan for care. A strong treatment plan shows how assessment findings, diagnosis, and the client’s priorities come together to guide therapy. When intake information is organized well, goals are clearer, interventions are intentional, and documentation supports both ethical practice and insurance requirements. This is what keeps the “golden thread” intact from assessment through ongoing sessions.
Mentalyc supports this process by helping therapists turn intake documentation into treatment plans that stay accurate over time. By pulling key clinical details from intake notes, suggesting SMART goals, and keeping plans aligned as progress notes are added, Mentalyc reduces documentation friction without taking over clinical judgment. The result is clearer treatment direction, stronger continuity of care, and documentation that reflects how therapists actually think and work.
Frequently Asked Questions (FAQs): How to Turn Intake Notes into a Treatment Plan
How do you turn intake notes into a treatment plan?
To turn intake notes into a treatment plan, clinicians synthesize assessment data into a diagnosis-driven structure that includes prioritized problems, client-centered goals, SMART objectives, and appropriate interventions. The treatment plan should clearly show how intake findings inform the course of therapy.
What is the intake to treatment plan workflow in therapy?
The intake to treatment plan workflow involves reviewing intake documentation, developing a clinical formulation, establishing a diagnosis, identifying key problem areas, and translating them into structured goals, objectives, and interventions that guide ongoing care.
Why is intake assessment synthesis important for treatment planning?
Intake assessment synthesis ensures that treatment plans are based on clinical interpretation rather than copied information. It helps connect symptoms, functional impairment, and diagnosis to meaningful goals and interventions, supporting medical necessity and continuity of care.
What makes a treatment plan insurance-ready?
An insurance-ready treatment plan includes a clear diagnosis, documented medical necessity, measurable goals and objectives, defined interventions, and evidence of ongoing review. Alignment between intake notes, treatment plans, and progress notes is essential.
Can Mentalyc turn intake notes into a treatment plan automatically?
Yes. Mentalyc can turn intake notes and session recordings into comprehensive, actionable treatment plans. It generates SMART goal suggestions, supports diagnosis-driven planning, and maintains alignment across documentation while allowing full clinician customization.
How does Mentalyc maintain the “Golden Thread” in documentation?
Mentalyc keeps intake notes, treatment plans, and progress notes connected in one continuous clinical narrative. This ensures that goals remain aligned with assessment findings and evolve as therapy progresses.
Do treatment plans need to be updated over time?
Yes. Treatment plans should be reviewed and updated as clients make progress, goals are achieved, or new clinical information emerges. Dynamic, evolving treatment plans better reflect real clinical work and support defensible documentation.
Why other mental health professionals love Mentalyc

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)

“For anyone hesitant: this is a lifesaver. It will change your life, and you have more time to be present with your patients.”
Licensed Clinical Social Worker

“Do yourself a favor, make your life easier. I found Mentalyc to be one of the best tools that I’ve ever used.”
Licensed Marriage and Family Therapist