Writing treatment plans is a core clinical task but also one of the easiest places for clarity to break down. Therapists are expected to turn diagnostic assessments into measurable, insurance-ready plans that guide care and evolve with the client. In practice, plans often become generic, disconnected from sessions, or difficult to keep updated. This guide provides treatment plan examples by diagnosis, showing how to create symptom-driven, evidence-based treatment plans with clear goals, practical objectives, and clinically appropriate interventions. Each example reflects real-world documentation needs while staying grounded in sound clinical reasoning.
Key Components of Any Treatment Plan
| Component | What It Includes | Why It Matters |
|---|---|---|
| Patient Information & Assessment | Demographics, presenting concerns, psychosocial history, risk factors, strengths, and functional impairments | Provides clinical context for diagnosis and ensures treatment planning is grounded in a full biopsychosocial understanding |
| Diagnosis (DSM / ICD) | Formal DSM-5-TR and/or ICD-10 diagnosis linked directly to assessed symptoms | Establishes medical necessity and anchors goals and interventions in recognized diagnostic criteria |
| Long-Term Treatment Goals | Broad, outcome-focused goals targeting symptom reduction and functional improvement | Clarifies the overall direction of care and communicates intended clinical outcomes |
| Short-Term Objectives | Specific, measurable, and time-bound steps that support each long-term goal | Makes progress observable and supports outcome monitoring and insurance review |
| Clinical Interventions | Evidence-based techniques, therapeutic modalities, session frequency, and duration | Demonstrates clinical rationale and ensures interventions are appropriate for the diagnosis |
| Crisis / Safety Plan | Steps for managing risk, emergency contacts, warning signs, and coping strategies | Protects client safety and demonstrates responsible risk management |
| Consent & Confidentiality | Informed consent, treatment agreement, and documentation of confidentiality limits | Ensures ethical practice and compliance with legal and professional standards |
Common Diagnoses & Example Treatment Approaches
These treatment plan examples show what diagnosis-driven planning looks like in practice—from intake findings to actionable goals and interventions. In each example, you’ll see:
- How the diagnosis directly informs the treatment plan
- How goals and objectives stay measurable and clinically grounded
- How symptoms, goals, and interventions stay clearly connected
Generalized Anxiety Disorder (GAD) – Anxiety Treatment Plan Example
Diagnosis: Generalized Anxiety Disorder (DSM-5-TR)
Clinical Presentation: Excessive worry occurring most days, muscle tension, sleep disturbance, restlessness, GAD-7 score of 17 (severe)
Long-Term Goal
Reduce generalized anxiety symptoms and improve emotional regulation and daily functioning.
Short-Term Objectives
- Client will reduce self-reported anxiety severity from 8/10 to 4/10 within 6 weeks.
- Client will identify at least three primary worry triggers within 4 sessions.
- Client will practice a grounding or relaxation exercise daily for 10 minutes and track anxiety levels for 4 consecutive weeks.
Clinical Interventions
- Weekly Cognitive Behavioral Therapy (CBT) targeting cognitive distortions and worry cycles
- Psychoeducation on anxiety physiology and threat perception
- Relaxation techniques (diaphragmatic breathing, progressive muscle relaxation)
- Mindfulness-based skills for present-moment awareness
- Referral for psychiatric evaluation for SSRIs if symptoms remain severe
Clinical Rationale:
CBT is a first-line, evidence-based intervention for GAD. Goals focus on worry reduction and physiological regulation, not avoidance of stressors.
Major Depressive Disorder (MDD) – Depression Treatment Plan Example
Diagnosis: Major Depressive Disorder, Moderate to Severe (F32.2)
Clinical Presentation: Persistent low mood, anhedonia, fatigue, withdrawal, negative self-concept
Long-Term Goal
Improve mood stability and increase engagement in meaningful daily activities.
Short-Term Objectives
- Client will engage in one pleasurable or mastery-based activity daily for 2 weeks.
- Client will identify and challenge two negative automatic thoughts per session using CBT tools.
- Client will report a clinically significant reduction in depressive symptoms within 8 weeks.
Clinical Interventions
- Behavioral activation to increase activity and motivation
- Cognitive restructuring of depressive thought patterns
- Interpersonal Therapy (IPT) strategies when relational stressors contribute
- Coordination with psychiatry for antidepressant medication, if indicated
- Strength-based exploration to rebuild self-esteem
Clinical Rationale:
Depression treatment prioritizes behavioral engagement before insight. Measurable activity-based objectives support early momentum and symptom relief.
Substance Use Disorder – Substance Abuse/Dependence Treatment Plan Example
Diagnosis: Substance Use Disorder (Alcohol or Drugs), Moderate
Clinical Presentation: High-risk substance use, limited coping skills, relapse history
Long-Term Goal
Achieve and maintain sobriety while developing sustainable coping strategies.
Short-Term Objectives
- Client will maintain continuous abstinence for 90 days.
- Client will identify five high-risk triggers and corresponding coping strategies within 4 weeks.
- Client will attend at least three peer-support meetings per week for 8 weeks.
Clinical Interventions
- Weekly individual therapy using Motivational Interviewing (MI)
- Group therapy focused on relapse prevention
- Participation in 12-step or peer support programs (AA/NA)
- Medication-Assisted Treatment (MAT), when appropriate
- Development of a written relapse prevention plan
Clinical Rationale:
Substance use treatment requires a multidisciplinary approach. Goals emphasize both abstinence and skill development to reduce relapse risk.
Family Conflict / Adjustment Issues
Diagnosis: Adjustment Disorder with Family Conflict
Clinical Presentation: High-conflict interactions, poor communication, emotional reactivity
Long-Term Goal
Improve family communication and reduce conflict intensity and frequency.
Short-Term Objectives
- Family will reduce verbal arguments to no more than once per week within 6 weeks.
- Family will establish and follow a weekly family meeting for 3 consecutive weeks.
- Each family member will demonstrate one effective communication skill per session.
Clinical Interventions
- Family systems therapy
- Communication and conflict-resolution skills training
- Structured family meeting agenda and rules
- Behavioral contracts and role clarification
Clinical Rationale:
Family conflict is maintained systemically. Interventions focus on interaction patterns, not individual blame.
PTSD Treatment Plan Examples
Diagnosis: Post-Traumatic Stress Disorder
Clinical Presentation: Intrusive memories, avoidance behaviors, hypervigilance, emotional numbing
Long-Term Goal
Reduce trauma-related symptoms and increase sense of safety and emotional regulation.
Short-Term Objectives
- Client will reduce avoidance behaviors by 50% within 8 weeks.
- Client will tolerate trauma-related discussion for 10–15 minutes per session without dissociation.
- Client will experience a 50% reduction in trauma-related nightmares within 3 months.
Clinical Interventions
- Trauma-Focused CBT (TF-CBT) or EMDR
- Stabilization and grounding skills
- Psychoeducation on trauma responses
- Gradual exposure or trauma processing once stabilization is achieved
Clinical Rationale:
Trauma treatment prioritizes safety and stabilization before processing to prevent re-traumatization.
OCD Treatment Plan Example
Diagnosis: Obsessive-Compulsive Disorder
Clinical Presentation: Intrusive thoughts, compulsive rituals, avoidance behaviors
Long-Term Goal
Reduce obsessive thoughts and compulsive behaviors to restore daily functioning.
Short-Term Objectives
- Client will reduce time spent on compulsions by 30% within 8 weeks.
- Client will complete one exposure with response prevention (ERP) exercise weekly.
- Client will identify their OCD cycle within 2 sessions.
Clinical Interventions
- Exposure and Response Prevention (ERP)
- Psychoeducation on OCD mechanisms
- Cognitive restructuring of threat beliefs
- Psychiatric consultation for SSRIs, if appropriate
Clinical Rationale:
ERP is the gold-standard treatment for OCD. Reassurance and avoidance are intentionally excluded from interventions.
ADHD Treatment Plan Example
Diagnosis: Attention-Deficit/Hyperactivity Disorder, Combined Presentation
Clinical Presentation: Inattention, disorganization, task initiation difficulty, emotional dysregulation
Long-Term Goal
Improve executive functioning and task completion across settings.
Short-Term Objectives
- Client will implement one organizational system within 2 weeks.
- Client will complete 70% of assigned tasks weekly for one month.
- Client will identify emotional triggers related to overwhelm within 4 sessions.
Clinical Interventions
- ADHD-focused skills coaching
- Behavioral strategies for task initiation and follow-through
- Psychoeducation on executive functioning
- Medication coordination, if indicated
Clinical Rationale:
ADHD treatment emphasizes external supports and skill development, not insight-only approaches.
Why Treatment Plans Often Break Down Over Time
Even thoughtfully written treatment plans can lose effectiveness as therapy progresses. The issue is rarely clinical skill—it’s structural.
Most treatment plans break down when:
1. Goals aren’t revisited regularly
As sessions evolve, new themes emerge and symptoms shift. When goals remain static, the plan no longer reflects the client’s current clinical needs or treatment focus.
2. Progress isn’t clearly tracked
Without a consistent way to see symptom change over time, therapists are forced to rely on memory or narrative notes. This makes it harder to evaluate what’s working, adjust interventions, or demonstrate measurable outcomes.
3. Documentation becomes disconnected from sessions
Intake notes, progress notes, and treatment plans often live in separate silos. When they aren’t actively linked, the Golden Thread breaks—leaving plans that feel generic and disconnected from real session work.
In practice, keeping treatment plans current requires 30–45 minutes of manual updating—time most clinicians simply don’t have. As a result, plans are updated infrequently, often right before an insurance review, rather than evolving naturally alongside treatment.
Mentalyc addresses this exact problem by keeping goals, progress, and session notes continuously connected—so treatment plans stay clinically accurate, measurable, and up to date without added administrative burden.
How Mentalyc Supports Diagnosis-Driven Treatment Planning
Diagnosis-driven treatment planning depends on one thing staying intact over time: the clinical logic connecting diagnosis, symptoms, goals, interventions, and progress. In real practice, that connection often breaks as documentation grows fragmented. Mentalyc supports diagnosis-driven planning by keeping those elements connected, directly from session documentation, without adding extra steps or administrative work.
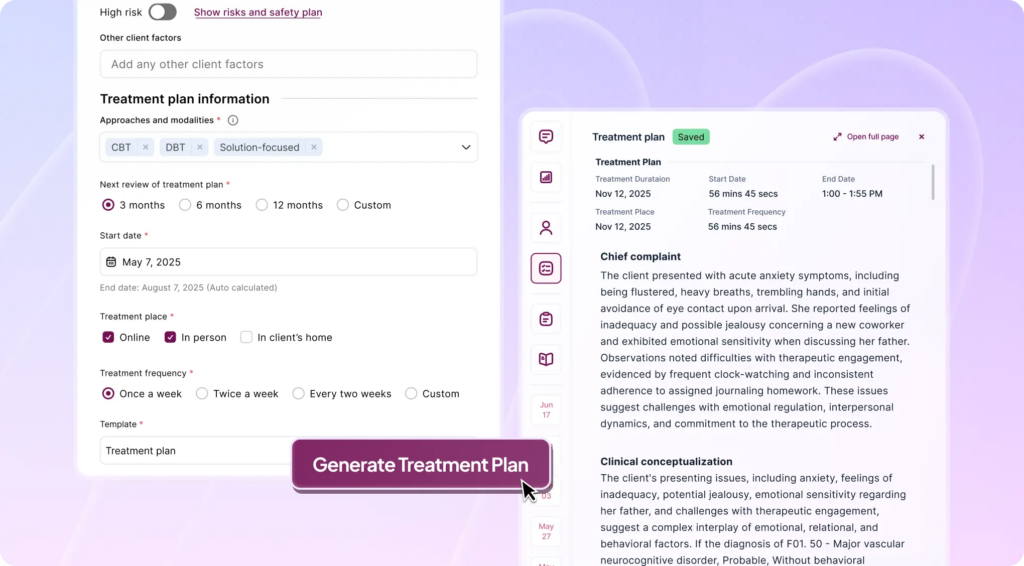
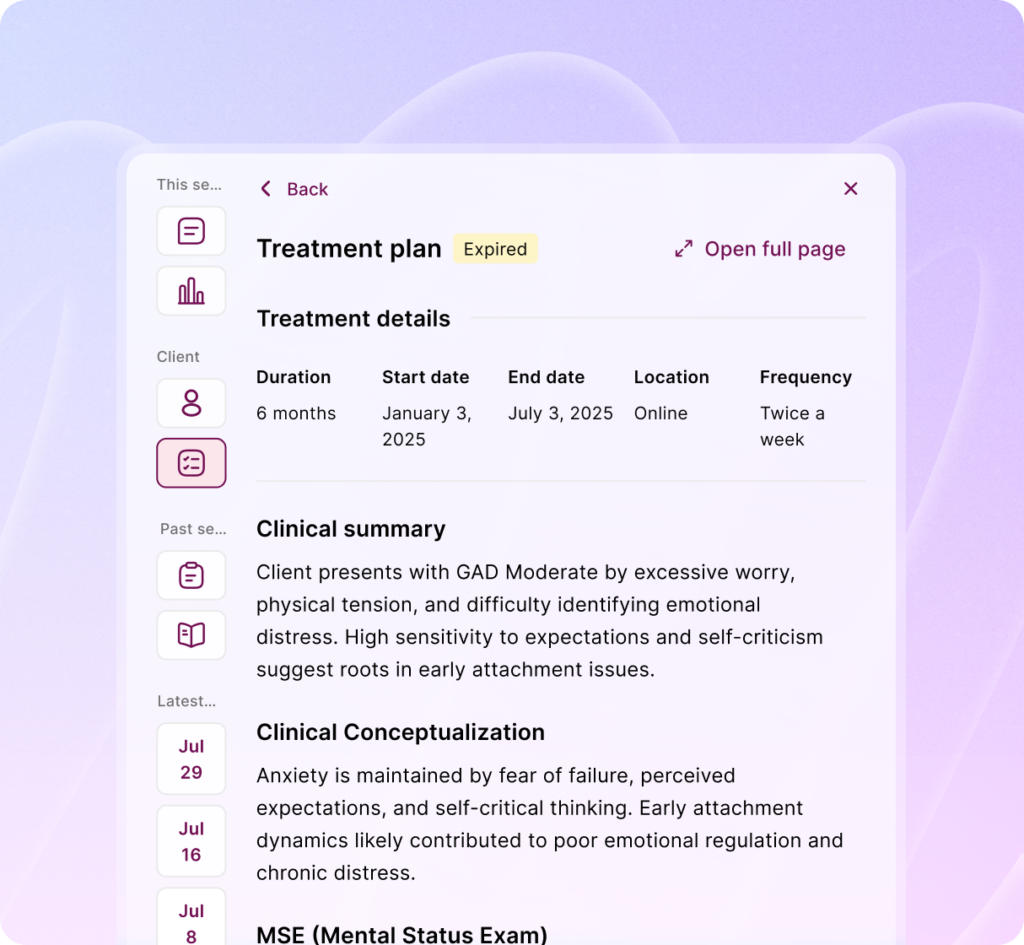
Treatment Plans Built Directly From Clinical Notes
Mentalyc’s AI Treatment Planner builds treatment plans directly from intake and progress notes. Documented symptoms, clinical observations, and presenting problems become the foundation of goals and objectives, ensuring plans reflect the diagnosed condition rather than generic templates. This keeps treatment planning aligned with DSM-informed documentation and medical necessity requirements.
Diagnosis-Aligned Goals That Stay Clinician-Controlled
From documented symptoms, Mentalyc suggests structured, measurable goals that clinicians can fully edit, refine, or replace. Goals remain linked to the diagnosis and evolve as symptoms change—without forcing rigid language or fixed timelines. The clinician’s judgment stays in the lead; our AI goal suggestions simply reduce setup time. You retain full clinical control:
- Edit language to match your voice
- Adjust baselines, targets, and timelines
- Remove or add goals as clinically appropriate
This makes goal setting faster without compromising clinical judgment.
Progress Tracking That Reinforces the Diagnosis
As sessions continue, Mentalyc’s AI Progress Tracker tracks symptom-related change directly from documented notes. This allows clinicians to see whether treatment is effectively addressing the diagnosed condition—without relying on separate forms or questionnaires. Progress becomes part of the treatment plan itself, not a disconnected reporting task.
Golden Thread Continuity Across Care
By linking intake assessments, treatment plans, progress notes, and symptom trends, Mentalyc maintains the Golden Thread required for clinical clarity, supervision, and insurance review.
Diagnosis-driven planning stays visible, defensible, and current—rather than static paperwork that quickly falls out of sync with real therapy work.
In practice: Mentalyc helps clinicians move from diagnosis → goals → interventions → outcomes as one continuous clinical story, grounded in session data and guided by professional judgment.
Ethical, Secure, and Clinically Responsible AI
Mentalyc is built for real clinical environments, with privacy and ethics at the core:
- Fully HIPAA, PHIPA, and SOC 2 Type II compliant
- No recordings stored
- No client data used for model training
- Custom BAA available for practices
This ensures diagnosis-driven treatment planning remains both clinically sound and ethically responsible.
Conclusion
Effective treatment plan examples are built on diagnosis-specific treatment plans, clear symptom driven goals, and evidence-based treatment planning that stays aligned over time. When goals, interventions, and progress remain connected to real session work, treatment plans guide care instead of becoming static paperwork. Mentalyc creates treatment plans by turning session insights into measurable goals, automatically tracking progress, and maintaining the Golden Thread across intake, treatment plans, and progress notes. The result is clinically accurate, insurance-ready documentation that evolves with your clients—without added administrative burden.
Frequently Asked Questions (FAQs) about Treatment Plan Examples
1. What makes a treatment plan diagnosis-specific?
A diagnosis-specific treatment plan directly links DSM-5-TR diagnostic criteria to the client’s presenting symptoms, goals, and interventions. Rather than using generic goals, the plan targets symptom patterns unique to the diagnosis, ensuring clinical relevance and medical necessity.
2. How detailed do treatment plan goals need to be for insurance?
Goals should be broad but measurable, while objectives should be specific and time-bound. Insurers typically look for:
- Clear symptom targets
- Measurable change over time
- Evidence that interventions align with the diagnosis
Well-structured SMART goals usually meet these requirements without excessive detail.
3. How often should treatment plans be updated?
Treatment plans should be reviewed and updated whenever:
- Symptoms significantly change
- Goals are met or no longer relevant
- Treatment focus shifts
Best practice is to review plans every 30–90 days, or more frequently for higher-acuity cases.
4. Can one client have multiple treatment plans or goals?
Yes. Clients often present with comorbid diagnoses or multiple problem areas. Each diagnosis may require its own goals and interventions, as long as the plan clearly maps symptoms to goals and avoids contradictory treatment directions.
5. How do you track progress without questionnaires?
Progress can be tracked through:
- Symptom frequency and intensity noted in sessions
- Behavioral indicators (e.g., reduced avoidance, increased engagement)
- Client self-report documented consistently
Tools like Mentalyc’s AI Progress Tracker identify trends directly from session notes, eliminating the need for separate forms.
6. What’s the biggest reason treatment plans fail audits?
The most common issue is broken continuity—when intake notes, treatment plans, and progress notes don’t clearly align. Auditors want to see a logical clinical story over time, often referred to as the Golden Thread.
7. Are AI-generated treatment plans clinically acceptable?
AI-generated treatment plans are clinically acceptable when they are clinician-reviewed and edited. AI should function as a support tool—not a replacement for professional judgment. Final responsibility for diagnosis, goals, and interventions always remains with the clinician.
Why other mental health professionals love Mentalyc

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)

“For anyone hesitant: this is a lifesaver. It will change your life, and you have more time to be present with your patients.”
Licensed Clinical Social Worker

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“Do yourself a favor, make your life easier. I found Mentalyc to be one of the best tools that I’ve ever used.”
Licensed Marriage and Family Therapist