Therapists researching a Blueprint review are usually trying to answer one simple question: Blueprint the right tool for me?
For clinicians who rely on routine assessments to monitor symptoms and meet reporting requirements, it’s a familiar option; but one that also raises important questions about insight between sessions, workflow fit, and long-term clinical value.
In this review, we break down how Blueprint performs in real therapy settings including its features, pricing, strengths, and limitations; and explain when it works well, when it falls short, and how it compares to alternative approaches to progress tracking in 2026.
Overview: What Is Blueprint?
Blueprint is an AI-powered outcomes and documentation platform designed for mental health clinicians who want to streamline clinical documentation, monitor progress, and incorporate measurement-based care into everyday practice.
The platform combines:
- Patient-reported outcome measures (PROMs) such as PHQ-9 and GAD-7
- AI-assisted therapy notes and treatment plans
- Session transcription and summaries
- Outcome dashboards to support evidence-based care
Blueprint is primarily built for clinicians that relied on standardized progress monitoring without adopting a full behavioral health EHR.
Key Takeaways — Blueprint Review 2026
| Area | Summary |
|---|---|
| What Blueprint does well | AI-assisted progress notes, structured treatment-plan drafting, PROM-based outcome tracking |
| Main limitations | Per-session pricing scales quickly for high-volume clinicians; EHR integration depth varies |
| Best practice fit | Solo clinicians and small teams using outcome measures and structured workflows |
| Privacy & compliance | HIPAA , PHIPA, SOC 2 Type II; audio processed temporarily, transcripts retained |
| Pricing model | Per-session (from ~$0.49/session); flexible for light caseloads |
| Best value for | Therapists prioritizing measurement-based care and quick documentation without a full EHR |
Who Blueprint Is Best For
Blueprint is best suited for clinicians who rely primarily on standardized outcome measures rather than session-level clinical insight:
- Solo clinicians who want lightweight progress tracking without adopting a full EHR
- Small to mid-size practices that prioritize structured assessment workflows over qualitative session analysis
- **CBT-oriented or outcomes-driven clinicians** who routinely use PROMs like PHQ-9, GAD-7, or ORS/SRS
Blueprint is less suitable for therapists who want to understand progress between assessments, track alliance dynamics, or connect session content directly to treatment goals.
Blueprint Mental Health Software Review — Real Blueprint Therapist Experience
Many therapists appreciate Blueprint’s automated documentation workflow, but some report challenges with transcription accuracy and note reliability, particularly when sessions involve nuanced dialogue or frequent back-and-forth between therapist and client.
A recurring theme in user feedback is the amount of post-session editing required to correct attribution errors or restore missing clinical detail.
One clinician described difficulty with speaker identification during live recording:
“My words often get mixed up for the client’s words… the transcript said there was a third person in the room when there definitely wasn’t.” — Ube Peafowl, via Blueprint Feedback Portal
Others note that while Blueprint reliably lists interventions, core clinical meaning can get diluted or repeated, requiring substantial manual revision:
“Often key content is lost or non-existent… I spend so much time editing.” — Apricot Cream Meadowlark, via Blueprint Feedback Portal
Taken together, these experiences suggest that Blueprint can accelerate the initial drafting of therapy notes, but note quality may vary depending on session complexity, recording clarity, and clinical style. For some clinicians, especially those with dense or relationally complex sessions, the time saved on drafting may be partially offset by the need for careful review and editing.
Blueprint Features — In-Depth Blueprint Mental Health Software Review
Blueprint positions itself as a measurement-based care platform with AI-assisted documentation features.
Blueprint Documentation Review
Automatic Note Generation
Blueprint captures session audio (or dictated summaries) and generates structured therapy progress notes and draft treatment plan content for clinician review.
Note Formats Supported
- SOAP, DAP, BIRP, GIRP
- Structured notes adaptable to modalities such as EMDR
- Other structured behavioral health formats via Chrome extension
Clinical Language & Accuracy
Blueprint still requires users make edits to generate notes. While output quality is generally strong, clinicians remain responsible for:
- Clinical accuracy
- Risk documentation
- Medical necessity language
As with all AI therapy documentation tools, review and sign-off are essential.
Editing & Customization
- Section-level regeneration tools
- Saved note preferences (length, tone, structure)
- Side-by-side transcript, summary, and note view via Chrome extension
Speed & Workflow
Blueprint emphasizes speed — often generating notes in under a minute. The workflow typically follows:
Record → Review → Light Edit → Copy into EHR
This keeps Blueprint lightweight but still dependent on manual EHR transfer for many users.
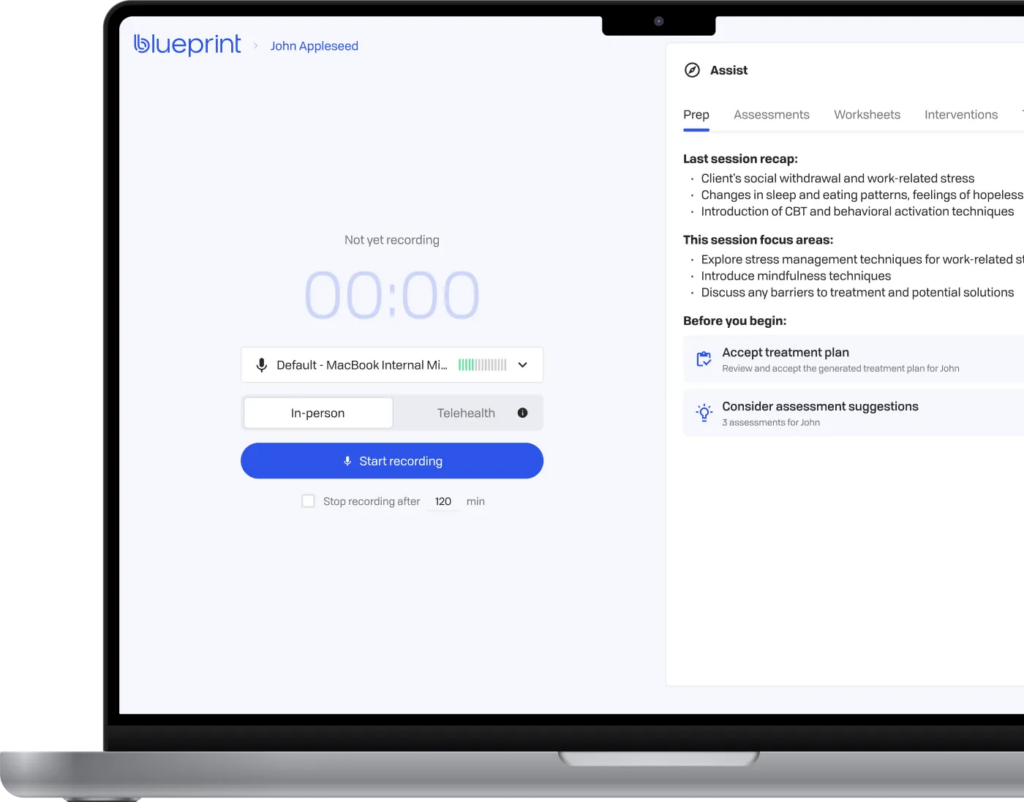
Blueprint Recording & Transcription Workflow
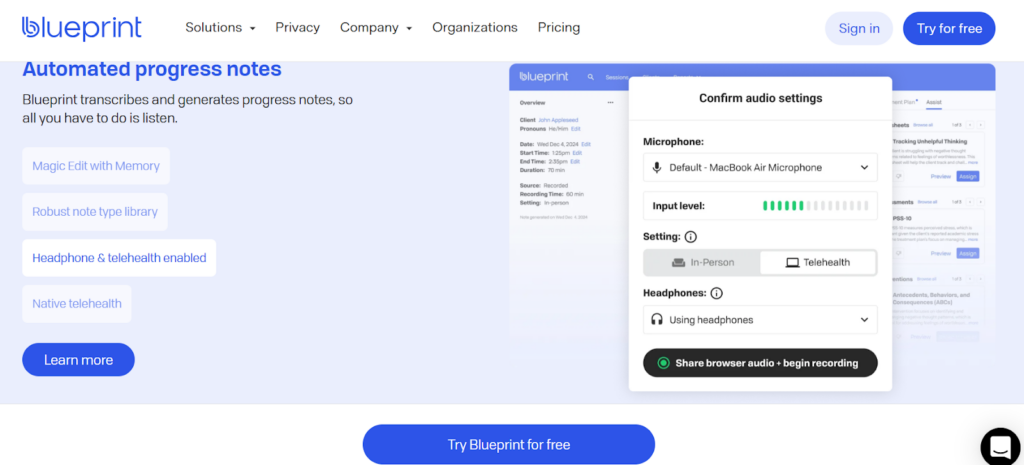
Session Capture Options
- Live recording (in-person or telehealth)
- Dictated summaries
- Uploaded audio or video files
- Browser-based capture via Chrome extension
- iOS mobile app
Transcription and Note Generation
Sessions are transcribed automatically, then converted into notes and (optionally) treatment plans.
Recording Storage
- Audio is processed temporarily and deleted after transcription
- Video is not stored
- Transcripts and notes remain encrypted within Blueprint
Clinicians must still use clear informed consent, especially when recording sessions.
Analytics, Insights & Outcome Tracking
Blueprint blends AI documentation with measurement-based care.
Session Insights
Blueprint surfaces high-level themes and summaries tied to session content. Public documentation confirms insight generation but does not fully disclose internal scoring models.
Outcome Measures (PROMs)
Blueprint has strong heritage in:
- PHQ-9, GAD-7, and validated instruments
- Symptom trend tracking over time
- Benchmarking improvement and remission rates
Progress Dashboards
Clinicians can:
- Monitor symptom changes
- Identify clients who are improving or plateauing
- Support outcome-focused supervision
Important distinction:
Blueprint’s progress tracking is primarily questionnaire-driven. This means progress visibility depends on when assessments are completed, rather than what unfolds between sessions.
If you specifically need fine-grained therapeutic alliance metrics or supervision-style feedback, you may need to compare Blueprint alternatives such as Mentalyc, which emphasize alliance and session-quality analytics more explicitly.
Collaboration & Group Practice Support — Blueprint Review
- Dedicated Supervision Note templates
- Organizational dashboards for multi-clinician practices
- Enterprise-level, score-based analytics for behavioral health organizations
Blueprint positions itself as a “clinical AI co-pilot” at the organizational level, particularly for systems focused on outcomes benchmarking.
Integrations & Workflow Support
- Designed to sit alongside existing behavioral health EHRs
- Structured notes copied into EHRs (not fully synced for most users)
- Includes built-in telehealth for session delivery.
- Telehealth video is not recorded or stored
Blueprint is not yet a full EHR replacement for most clinicians.
Security, Privacy & Compliance
Blueprint publicly states:
- HIPAA & PHIPA compliant
- SOC 2 Type II certified
- BAAs available
- AES-256 encryption at rest and in transit
- Audio deleted post-transcription
- Transcripts and notes encrypted and retained
Blueprint also provides client-consent guidance to support ethical AI use in therapy.
Blueprint Pricing (2026)
| Plan | Price | What’s Included | What’s NOT Included | Free Trial |
|---|---|---|---|---|
| Standard | $0.49/session | AI-generated notes, transcription, telehealth, basic documentation tools | No advanced insights; limited clinical decision support | 5 free sessions |
| Plus | $0.99/session | Everything in Standard + enhanced clinical insights & decision support | No full EHR admin (billing, intake, scheduling) | 5 free sessions |
| Pro (Coming Soon) | $1.49/session | Automated notes + insights + full AI-assisted EHR (intake, billing, payments, scheduling) | Not available yet; features still rolling out | Not announced |
| Enterprise | Custom | API access, deeper EHR integrations, volume discounts, org-level tools | Depends on contract; may require minimum volume | No |
Pricing Insight
- Cost-effective for clinicians with low or fluctuating session volume
- Becomes more expensive than flat-rate tools as session volume increases
H2: Blueprint Pros & Cons
Pros
- Offers AI-generated notes and draft treatment-plan content
- Provides PROM-based outcome tracking (PHQ-9, GAD-7, ORS/SRS)
- Multiple session capture options (recording, dictation, uploads)
Cons
- Progress visibility depends on client-completed questionnaires rather than session content
- Limited insight into session-to-session change, alliance dynamics, or in-session progress
- Notes and outcomes are not natively connected to treatment goals over time
- Documentation often requires manual transfer into a separate EHR
H2: Final Verdict: Is Blueprint Worth It for Therapists in 2026?
Blueprint is a good fit for therapists who rely on standardized outcome measures and want a structured way to track symptoms without adopting a full EHR.
It works best for solo clinicians and small practices using questionnaires like PHQ-9 or GAD-7 to monitor change. Its main limitations are that progress tracking depends on client-completed forms, and treatment plans tend to function as static documents rather than tools that stay closely connected to what happens in session.
Therapists who want notes, goals, and progress to stay closely aligned over time — with clearer visibility into how sessions are contributing to change — may want to explore other options built around session-based insight rather than periodic assessments.
H2: Best Alternatives to Blueprint
H3: Mentalyc — Best for fully automated, insight-driven documentation
Why choose Mentalyc?
Mentalyc helps therapists create accurate clinical notes and track progress directly from each session — without questionnaires or extra admin work. Notes, treatment plans, and progress stay connected, making it easier to see how clients are moving through treatment over time.
What sets Mentalyc apart:
- Generates notes and treatment plans from session recordings, uploads, dictation, or summaries
- Supports documentation across care settings, including individual, couples, family, and group therapy, as well as psychiatry workflows.
- Produces structured, audit-ready documentation that supports insurance reviews and continuity of care
- Keeps intake notes, session notes, goals, and progress clearly linked over time
- Includes an AI Progress Tracker that shows symptoms change based on session content — no questionnaires required
- Offers Alliance Genie™, a unique feature that highlights therapeutic alliance patterns and relational signals
- Built with a privacy-first approach (HIPAA, PHIPA, BAA SOC 2; no recording storage)
Other alternatives
- Upheal — notes + analytics with questionnaire-based tracking
- Supanote / AutoNotes — simple note-writing efficiency tools
H2: Quick Comparison: Blueprint Vs Mentalyc

| Feature | Blueprint | Mentalyc |
|---|---|---|
| Automation level | AI-assisted documentation: records or transcribes sessions and drafts notes and treatment plans for clinician review and editing. | Highly automated documentation that generates notes and treatment plans from audio, uploads, dictation, or typed summaries with minimal clinician editing. |
| Clinical accuracy | Generally strong structured output, but accuracy can vary based on transcription quality and session complexity; clinician review is essential. | Mental-health-specific system producing clinically relevant, insurance-ready notes with consistent alignment across documentation, treatment plans, and progress (the “golden thread”). |
| Note types | Supports common formats (SOAP, DAP, BIRP, GIRP, EMDR-style) but not all client types. | Supports all client types with a broad clinical template library including SOAP, DAP, BIRP, PIRP, GIRP, PIE, SIRP, intake notes, group and family sessions, and SMART treatment plans. |
| Progress tracking | Relies on patient-reported outcome measures (e.g., PHQ-9, GAD-7) with limited automation beyond scoring and graphing. | Tracks progress directly from session notes and treatment goals—no client questionnaires required. |
| Alliance insights | No alliance insights metric. | Alliance Genie™ provides structured therapeutic-alliance analysis and supervision-style insights (unique to Mentalyc). |
| Recording storage | Audio processed temporarily for transcription and deleted; transcripts and notes stored encrypted. | Audio processed temporarily for transcription and deleted; transcripts stored securely and never used for model training. |
| HIPAA / SOC 2 | HIPAA & PHIPA compliant, SOC 2 Type II certified; BAAs available. | HIPAA & PHIPA compliant, SOC 2 Type II compliant; BAAs available with a privacy-first design. |
| Pricing | Per-session pricing (from ~$0.49/session); costs increase with higher caseload volume. | Flat monthly plans with note limits—more predictable for steady or high-volume caseloads. |
| Best for | Clinicians relying on measurement-based care with standard PROMs and questionnaire-driven outcome tracking. | Clinicians seeking automated, privacy-first documentation with session-based progress tracking and alliance insights. |
To learn more, check this detailed Blueprint vs Mentalyc comparison.
H2: FAQs: Blueprint Review and Best Blueprint Alternatives
H3: Is Blueprint HIPAA compliant?
Yes. Blueprint’s HIPAA compliance is clearly stated on its security page: the company reports that it is HIPAA and PHIPA compliant, SOC 2 Type II audited, uses 256-bit encryption, and offers a Business Associate Agreement (BAA) for covered entities.
H3: Does Blueprint store therapy recordings?
Blueprint states that it does not store audio recordings of sessions. Audio is captured to power the Blueprint transcription and note-generation workflow, then “processed and discarded in real time.” However, the transcription file and generated Blueprint therapy notes are stored on Blueprint’s servers, encrypted and protected under HIPAA and SOC 2 Type II controls.
H3: Are AI tools safe for clinical documentation?
AI tools can be used safely for clinical documentation if several conditions are met:
The vendor is HIPAA/PHIPA compliant, offers a BAA, uses strong encryption, and has independent security audits (e.g., SOC 2 Type II).
The tool provides transparent information on data usage, retention, and whether data is used for model training.
Clinicians review, edit, and sign off on every AI-generated note and never treat AI output as a substitute for independent clinical judgment. Even with compliant tools like Blueprint, AI can miss nuance or introduce subtle inaccuracies, so the therapist remains responsible for ensuring clinical accuracy, risk documentation, and payer compliance before finalizing notes.
H3: What note types does Blueprint support?
Blueprint is built specifically for behavioral health and supports the most common therapy note formats. Its clinical education and product materials highlight templates and examples for:
- SOAP notes
- DAP notes
- BIRP notes
- GIRP, PIRP, PIE, and case-management style notes
- Audit-ready progress notes and treatment plans that follow these frameworks.
Within the app and Chrome extension, Blueprint uses these structures to generate structured therapy notes, which clinicians can then customize to match payer or agency standards.
H3: What are the best alternatives to Blueprint?
If you’re exploring best alternatives to Blueprint, a few tools stand out—Mentalyc in particular for clinicians who want insight beyond questionnaires.
Mentalyc
- Drafts clinically aligned progress notes and SMART treatment plans from session audio, uploads, dictation, or short summaries, reducing the need for repetitive manual editing.
- Offers session-derived progress tracking, where change is reflected directly from clinical notes and treatment plans—not only from PROMs or self-report measures.
- Includes Alliance Genie™, which surfaces patterns related to therapeutic alliance, engagement, and session flow to support reflection, supervision, and clinical decision-making.
- Mental health–specific platform built for therapists, emphasizing continuity across notes, treatment plans, and progress (the “golden thread”).
- Privacy-first by design, with HIPAA, PHIPA, and SOC 2 Type II compliance to support secure, audit-ready documentation and longitudinal tracking.
Upheal
AI progress notes and treatment plans with Golden Thread documentation, detailed analytics, and multi-language support for mental health providers.
Supanote or AutoNotes
Both offer AI-generated SOAP/DAP/BIRP-style notes with straightforward pricing and are often listed in independent “AI therapy documentation tools” and Blueprint alternatives roundups.
For many clinicians, Blueprint is a strong choice for AI-assisted documentation plus outcome tracking, while Mentalyc is often preferred when you want fully automated notes, a mental-health-only focus, privacy-first design, and a very strong golden thread across your documentation.
Why other mental health professionals love Mentalyc

“Do yourself a favor, make your life easier. Use the tools that are readily available … I found Mentalyc to be one of the best tools that I’ve ever used.”
Licensed Marriage and Family Therapist

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“It immediately changed my quality of life, personally and professionally. I went from 3–4 hours a week of notes to 1 hour at most … that alone is invaluable personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (IMFT)

“For those who have hesitations … It is a lifesaver. It will change your life and you have more time to be present with your patients.”
Licensed Clinical Social Worker