Therapy is not just about what you work on — it’s about when and how you work on it. One of the most common reasons treatment stalls or feels unfocused is not lack of skill or effort, but unclear goal sequencing in therapy. This is where understanding short term vs long term therapy goals becomes essential.
Short-term goals give clients relief, safety, and momentum. Long-term goals give therapy meaning, depth, and lasting change. When these are confused, rushed, or poorly connected, therapy can feel chaotic — for both the clinician and the client. This guide breaks down how short term therapy objectives and long term treatment goals differ, how they support each other, and how clinicians can use phased therapy goal planning to create a clear, flexible therapeutic roadmap that holds up clinically and administratively.
Long Term vs Short Term Therapy Goals: Core Differences
| Dimension | Short-Term Goals | Long-Term Goals |
|---|---|---|
| Time horizon | Days to weeks | Months to years |
| Focus | Symptoms & skills | Patterns & meaning |
| Scope | Specific & concrete | Broad & integrative |
| Function | Stabilization | Transformation |
| Measurement | Observable change | Sustained life impact |
Common Mistakes Clinicians Make With Therapy Goals
Even experienced clinicians can run into challenges when setting or managing therapy goals. These issues usually aren’t about skill; they’re about how goals are structured and revisited over time. Below are some of the most common pitfalls and why they can interfere with effective treatment.
1. Treating All Goals as Equal
Not all goals belong in the same stage of therapy. Immediate safety or stabilization goals require a different focus than long-term identity or relational work.
When short-term crisis goals are mixed with deeper, long-term change goals, clients may feel overwhelmed or confused about what therapy is actually trying to accomplish. Clinically, this can lead to misaligned expectations and frustration on both sides.
Separating goals by phase helps therapy feel more focused and achievable.
2. Confusing Interventions With Goals
A common source of confusion is using techniques or activities as goals.
- Goal: Reduce panic-related avoidance
- Intervention: Gradual exposure exercises
Goals describe what needs to change.
Interventions describe how you work toward that change.
When interventions are written as goals, it becomes difficult to evaluate progress or explain clinical reasoning—especially in documentation or insurance review. Clear goals keep treatment direction understandable and defensible.
3. Overloading Treatment Plans
Including too many goals at once can dilute clinical focus. When everything is a priority, it becomes hard to track meaningful change or know what to adjust.
Clinically, it’s often more effective to focus on one primary change per goal, supported by related interventions. This allows progress to be observed more clearly and helps clients experience momentum rather than overwhelm.
4. Failing to Revisit and Update Goals
Therapy goals should evolve as clients gain insight, stability, or new challenges emerge. When goals remain unchanged for long periods, they can lose relevance to the client’s current experience.
From a clinical perspective, outdated goals can:
- Disconnect sessions from treatment direction
- Reduce client engagement
- Create gaps in documentation clarity
Regularly revisiting goals helps ensure that therapy stays responsive, intentional, and aligned with both clinical needs and external review requirements.
What Are Short-Term Therapy Goals?
Short-term therapy goals focus on what needs attention right now. They are practical, near-term objectives that help stabilize symptoms, build basic coping skills, and make it possible for clients to engage more fully in therapy. Rather than aiming for deep or lasting change immediately, short-term goals create a sense of safety and forward movement. They help reduce distress, bring some structure to the client’s experience, and establish early signs that therapy is helping.
In simple terms, short-term goals address the question: “What does this client need in the next few weeks to feel steadier and able to do the work of therapy?”
Key Characteristics of Short-Term Goals
Short-term goals tend to share a few important features:
- Time-limited: Usually set for days or weeks, not months
- Present-focused: Address current symptoms, stressors, or functional difficulties
- Specific and narrow: Focus on one clear area rather than broad life change
- Stabilizing in nature: Support safety, regulation, and basic coping
These goals are meant to be realistic and achievable within a short window, even when a client is overwhelmed or in crisis.
Examples of Short-Term Therapy Objectives
Short-term goals often look like small but meaningful steps, such as:
- Reducing the frequency or intensity of panic attacks over the next few weeks
- Establishing a more consistent sleep or daily routine
- Learning and practicing grounding or calming techniques
- Increasing tolerance for strong emotions without shutting down or escalating
- Planning and having one difficult but necessary conversation
- Attending sessions regularly during a stressful period
Each goal is concrete and observable, making it easier to notice progress and adjust the approach if needed.
Clinical Purpose of Short-Term Goals
Short-term goals serve several important functions in therapy:
- Reduce immediate suffering, making life feel more manageable
- Build emotional regulation, so clients are less reactive or overwhelmed
- Create momentum, helping clients experience early success
- Prepare clients for deeper work by increasing stability and trust
When short-term goals are missing, long-term therapeutic work can feel too abstract or intimidating. By focusing first on what’s most urgent and achievable, therapy becomes more accessible—and progress becomes easier to sustain.
What Are Long-Term Therapy Goals?
Long-term therapy goals focus on enduring psychological change rather than immediate symptom relief. They address the deeper patterns that shape how a client relates to themselves, others, and the world over time. These goals often involve identity, attachment, belief systems, emotional patterns, and long-standing ways of coping. Unlike short-term goals, long-term goals are not about quick fixes. They are about meaningful, lasting shifts that unfold gradually as therapy progresses.
In simple terms, long-term goals answer the question: “What kind of life does this client want to build — and what internal patterns need to change to support that?”
Key Characteristics of Long-Term Goals
Long-term therapy goals tend to share several defining features:
- Extended timeframe: Often months or years rather than weeks
- Pattern-focused: Address recurring emotional, relational, or cognitive themes
- Broad in scope: Involve identity, relationships, or core ways of being
- Integrative: Build on skills and insights developed earlier in therapy
- Nonlinear: Progress often includes setbacks, pauses, and revisions
These goals evolve as clients gain insight, stability, and new capacities.
Examples of Long-Term Treatment Goals
Long-term goals vary widely depending on the client and therapeutic approach, but common examples include:
- Processing and integrating unresolved trauma
- Developing secure, stable, and reciprocal relationships
- Building a consistent sense of self-worth and identity
- Changing deeply ingrained cognitive or relational patterns
- Maintaining emotional stability across changing life circumstances
- Developing greater self-compassion and psychological flexibility
These goals are rarely achieved through a single technique or insight. Instead, they emerge through sustained therapeutic work over time.
Clinical Purpose of Long-Term Goals
Long-term goals serve as the directional compass of therapy. They help:
- Give therapy a sense of meaning beyond symptom reduction
- Guide clinical focus as sessions and priorities shift
- Connect day-to-day work to deeper transformation
- Support sustained change rather than short-term improvement
- Help therapists and clients understand why the work matters
When long-term goals are clear, therapy becomes more cohesive. Even short-term interventions such as coping skills or symptom stabilization can be understood as steps toward broader, lasting change.
How Short-Term and Long-Term Goals Work Together

Effective therapy is rarely about chasing isolated goals. Instead, it relies on a goal hierarchy, where short-term goals support longer-term change over time. Short-term and long-term goals are not competing priorities. They work best when they are clearly connected.
Short-Term Goals as Building Blocks
Clients rarely reach long-term outcomes—like healing trauma or changing entrenched patterns—in one leap. Change happens in stages.
For example, before a client can process trauma meaningfully, they often need to:
- Learn basic emotional regulation
- Increase a sense of safety and stability
- Build tolerance for distress
- Develop insight into patterns and triggers
- Begin integrating meaning and new narratives
Each of these steps represents a short-term goal. On its own, a short-term goal may seem modest, but together they create the conditions necessary for lasting change. Short-term goals make progress feel possible and keep therapy grounded in what the client can realistically work on right now.
Long-Term Goals as A Fluid, Dynamic Process
Therapy goals are not fixed. As symptoms decrease, different challenges often emerge. As insight grows, priorities shift. What mattered early in treatment may no longer be the most relevant focus months later. Hence, effective treatment timeline planning depends on ongoing reflection, not just an initial treatment plan. Therapists need to see how session work is unfolding over time so they can adjust goals without losing direction.
This is where tools like Mentalyc Treatment Planner can be helpful. By tracking patterns, symptoms, and themes across sessions, Mentalyc makes it easier to notice when short-term goals are being met, when they need to change, and how they connect to longer-term aims, without relying on extra forms or constant plan rewrites.
The Best Approach to Goal Setting? Balanced Care with Immediate Needs and Long-Term Direction
Strong treatment planning balances three things at once:
- Addressing immediate symptoms or stressors
- Keeping sight of deeper, long-term change
- Allowing flexibility as the client evolves
When this balance is missing, therapy can start to feel either reactive, only responding to crises or vague, with no clear sense of progress. When goals are connected and revisited over time, therapy feels more coherent and intentional.
By helping therapists see how day-to-day session work accumulates into meaningful patterns, Mentalyc supports this balance—making it easier to align short-term interventions with long-term therapeutic direction, while keeping clinical judgment firmly in control.
Phased Therapy Goal Planning: A Clinical Framework
Effective therapy rarely follows a straight line, but it does follow a sequence. Phased therapy goal planning organizes treatment into intentional stages that reflect a client’s readiness, capacity, and clinical needs; rather than treating all goals as equally urgent or appropriate at the same time.
Instead of a flat list of goals competing for attention, phased care planning creates order, pacing, and clinical rationale. It helps therapists answer a critical question throughout treatment:
“What kind of work is appropriate for this client right now?”
Phase 1: Stabilization & Safety
Primary focus: symptom reduction, coping, and safety
Phase 1 is about helping the client function well enough to participate in therapy. When clients are overwhelmed, dysregulated, or in crisis, deeper exploratory work is not just ineffective—it can be harmful.
In this phase, goals prioritize immediate relief and stabilization, not long-term transformation.
Typical goals include:
- Crisis management and safety planning
- Emotional regulation and distress tolerance
- Improving sleep, appetite, and daily routines
- Reducing acute symptom intensity or frequency
The clinical aim is to help the nervous system settle and restore a sense of predictability. These short term therapy objectives create the foundation for everything that follows. Without adequate stabilization, insight-oriented or trauma-focused work often leads to avoidance, dropout, or symptom worsening.
Phase 1 answers the question: “Is this client stable enough to go deeper?”
Phase 2: Skill Development & Insight
Primary focus: patterns, awareness, and relational dynamics
Once clients have sufficient regulation and safety, therapy can shift toward understanding why problems persist and how patterns are maintained. This is where goal sequencing in therapy becomes especially important.
In Phase 2, goals expand beyond symptom control to include meaning-making and behavioral change.
Typical goals include:
- Identifying cognitive distortions and maladaptive beliefs
- Recognizing emotional and behavioral patterns
- Improving communication and relational boundaries
- Building emotional literacy and self-reflection
Here, short-term goals often involve practicing new skills or experimenting with different responses, while long term treatment goals begin to take clearer shape. Clients start to see how present-day difficulties connect to past experiences, attachment patterns, or core beliefs.
Phase 2 answers the question: “What patterns are driving this client’s difficulties?”
Phase 3: Integration & Maintenance
Primary focus: sustainability, identity, and meaning
Phase 3 is about consolidation. The goal is not just improvement, but durable change that carries beyond the therapy room.
At this stage, therapy shifts from active intervention to integration—helping clients apply what they’ve learned across contexts and maintain gains over time.
Typical goals include:
- Maintaining progress across relationships, work, and stressors
- Strengthening self-concept and internalized coping
- Increasing autonomy and confidence in self-regulation
- Preparing for termination or reduced session frequency
Goals in this phase often focus on relapse prevention, values alignment, and future-oriented planning. Therapy becomes less about solving problems and more about supporting a coherent sense of self.
Phase 3 answers the question: “How does this client carry these changes forward independently?”
Why Phased Planning Works
This three-phase structure creates a therapeutic roadmap that both clinicians and clients can understand. It:
- Prevents premature deep work before stabilization
- Clarifies why certain goals come before others
- Supports ethical pacing and client readiness
- Makes progress easier to explain, track, and adjust
Phased therapy goal planning doesn’t lock therapy into a rigid formula. Clients may move back and forth between phases as life circumstances change. What it offers is clinical clarity—a way to ensure that each goal fits the client’s current needs while still moving treatment forward with intention.
In practice, phased care planning is what turns goals into a coherent treatment journey rather than a collection of disconnected tasks.
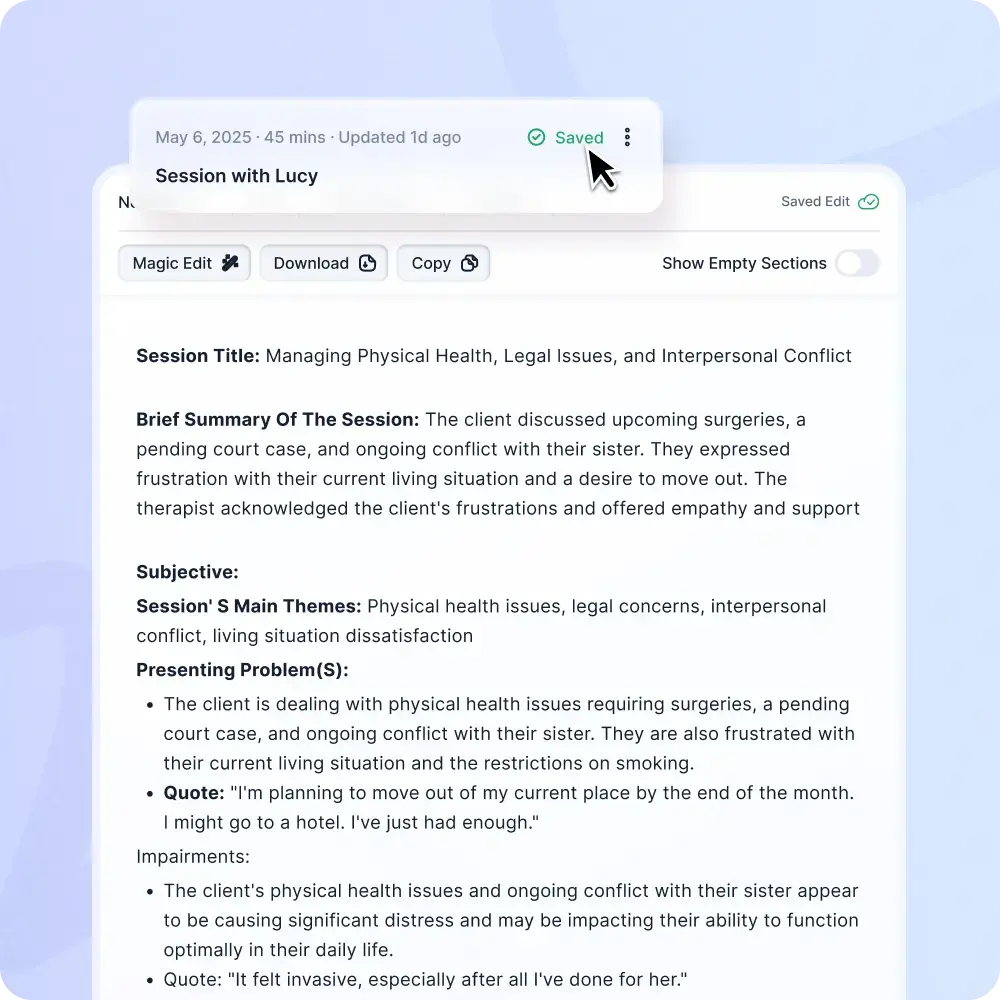
How Mentalyc Supports Short-Term and Long-Term Goal Planning
Designing short-term and long-term goals is a core clinical skill. The real challenge is keeping those goals aligned, measurable, and clinically relevant as therapy unfolds over time. In day-to-day practice, goals often drift away from session work, treatment plans go stale, and progress becomes difficult to explain or document.
Mentalyc is designed to support goal planning as an ongoing clinical process, not a one-time administrative task.
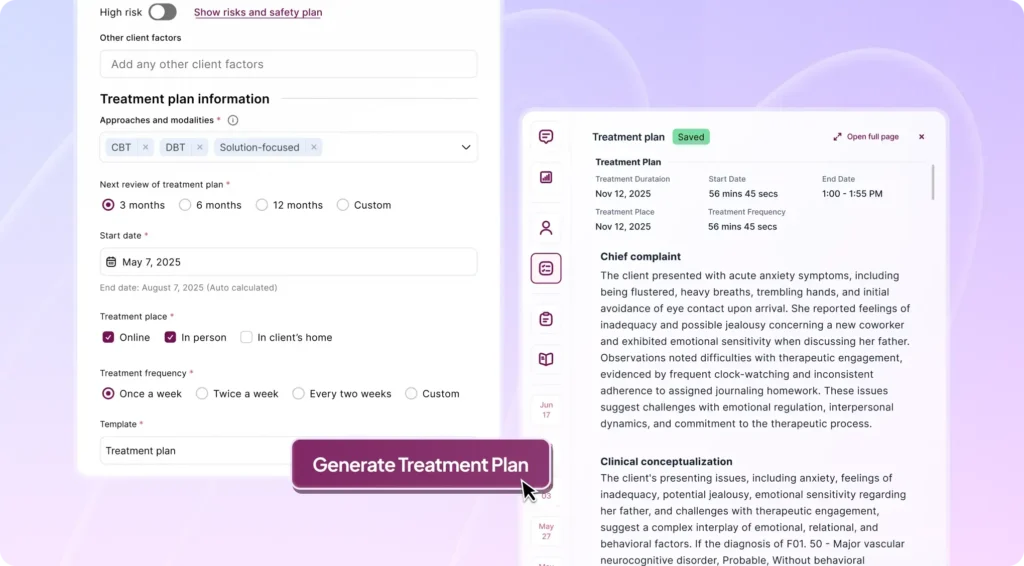
Turning Session Work Into Clear, Goal-Focused Plans
Mentalyc’s AI Treatment Planner begins with what already exists: your session notes.
Instead of requiring clinicians to manually translate clinical work into formal goals, Mentalyc analyzes session content to:
- Identify relevant symptoms, themes, and clinical focus areas
- Suggest SMART short-term therapy objectives that reflect what the client is actively working on
- Organize those objectives under broader long-term treatment goals
Because goals are generated directly from session material, they reflect real clinical thinking rather than generic templates. The language stays aligned with your modality, your interventions, and your client’s presentation.
Supporting Goal Hierarchy, Not Disconnected Objectives
Mentalyc structures treatment plans around goal hierarchy, which mirrors how therapy actually progresses.
- Long-term goals represent the overarching direction of care (e.g., sustained anxiety reduction, improved relational functioning, trauma integration).
- Short-term objectives sit beneath those goals as focused, time-bound steps that move treatment forward.
This structure makes it clear how early stabilization goals, skill-building work, and later integration efforts all connect. Instead of revisiting a flat list of goals every few months, clinicians can see how short-term progress is actively contributing to longer-term change.
Built for Phased Therapy Goal Planning
Therapy does not progress all at once, and Mentalyc is designed to reflect that reality. Mentalyc naturally supports phased care planning across the course of treatment. As sessions progress:
- Early-phase objectives (stabilization, regulation, safety) can be completed or de-emphasized
- Mid-phase objectives (insight, pattern change, relational skills) emerge from ongoing work
- Long-term goals remain visible while being refined as the client develops new capacity
Because Mentalyc updates the treatment plan as new session notes are added, goals stay clinically current without constant manual rewriting. The plan evolves alongside the client rather than lagging behind the work.
Progress Tracking Without Extra Forms or Scoring
Mentalyc tracks progress toward both short-term and long-term goals directly from session documentation. This allows clinicians to see whether short-term objectives are being met, understand how those changes support broader goals, and recognize when goals need adjustment. Progress is derived from the clinical material already captured in session notes, not from separate questionnaires or rating scales. The result is session-based, survey-free progress tracking that still supports measurable, insurance-ready documentation – without adding administrative work.
Maintaining the Golden Thread Across Care
Mentalyc keeps treatment plans, session notes, and progress tracking connected as one continuous clinical narrative. This makes it easier to adjust goals as clients change, demonstrate medical necessity, and stay aligned during supervision or insurance review. Instead of fragmented documents, clinicians have a coherent story of care that shows how goals, interventions, and outcomes relate over time.
Why This Matters in Practice
When short-term and long-term therapy goals are clearly structured and continuously updated:
- Sessions feel more focused and intentional
- Clients better understand how today’s work connects to longer-term change
- Therapists spend less time maintaining paperwork and more time doing therapy
Mentalyc supports goal planning the way therapy actually happens—iterative, phased, and grounded in real session work—so treatment plans remain useful clinical tools rather than static documents.
Conclusion: Short Term vs Long Term therapy Goals Are a Journey, Not a Checklist
Effective therapy is not about choosing between short-term or long-term goals. It’s about understanding how they work together. Short-term goals create stability and momentum. Long-term goals provide direction and meaning. When organized through phased goal planning, they form a therapeutic roadmap that adapts as clients grow. With the right structure and the right tools like Mentalyc, therapy goals become clearer, more coherent, and easier for both therapists and clients to trust.
FAQs: Long Term vs Short Term Therapy Goals
1. What is the difference between short term vs long term therapy goals?
Short-term goals focus on immediate symptom relief and skill-building, while long-term goals address deeper patterns, identity, and sustained well-being.
2. How many short-term therapy objectives should a client have at once?
Typically 1–3 active short-term objectives per phase to maintain focus and track progress effectively.
3. Can long-term treatment goals change during therapy?
Yes. Long-term goals often evolve as clients gain insight and their priorities shift.
4. What is phased therapy goal planning?
It’s an approach that organizes therapy goals into stages (stabilization, insight, integration) to match the client’s readiness and needs.
5. How do therapists track progress across long-term goals?
By linking short-term objectives to long-term outcomes and monitoring progress session by session.
6. Does Mentalyc support both short-term and long-term therapy goals?
Yes. Mentalyc’s AI Treatment Planner creates SMART goals, organizes them hierarchically, and tracks progress automatically across sessions.
7. Are Mentalyc treatment plans insurance-compliant?
Yes. Plans are structured, measurable, and aligned with documentation standards while remaining fully HIPAA & SOC 2 Type II compliant.
Why other mental health professionals love Mentalyc

“For anyone hesitant: this is a lifesaver. It will change your life, and you have more time to be present with your patients.”
Licensed Clinical Social Worker

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)

“Do yourself a favor, make your life easier. I found Mentalyc to be one of the best tools that I’ve ever used.”
Licensed Marriage and Family Therapist