In day-to-day practice, therapists are constantly assessing whether therapy is helping — often through clinical intuition, memory, and scattered documentation. Yet as cases extend over months or years, it becomes increasingly difficult to hold the full trajectory of change in mind. Symptom trend tracking in therapy brings those impressions into focus by showing how symptoms evolve across sessions, without turning therapy into a checklist exercise.
Rather than asking “Did the client meet a goal?”, symptom trend tracking answers a more clinically grounded question: How are the client’s symptoms actually changing over time?
This article takes a detailed look at symptom trend tracking, how it fits into real-world clinical work, common pitfalls to avoid, and how Mentalyc supports this process in a way that preserves nuance, judgment, and therapeutic integrity.
What Is Symptom Trend Tracking in Therapy?
Symptom trend tracking in therapy is the longitudinal observation of symptom changes across sessions, focused on how clinical indicators evolve rather than whether a specific target has been “met.”
Traditionally, symptom trend tracking has relied on manual symptom charts, tracking worksheets or PDFs, and periodic rating scales completed by clients or clinicians to monitor change over time. These tools are often used to capture symptom frequency, intensity, or distress levels between sessions. While useful, they typically require additional effort outside the session and can fragment the clinical narrative.
| Clinical Focus | What Is Tracked | Why It Matters |
|---|---|---|
| Symptom presence | Whether a symptom continues or resolves | Confirms clinical relevance |
| Frequency | How often the symptom occurs | Reflects functional impact |
| Intensity | How severe the symptom feels or presents | Signals distress level |
| Change over time | Direction and pattern across sessions | Reveals improvement or escalation |
While symptom trends are always interpreted through clinical judgment, tracking frequency and intensity over time provides a more objective reference point than memory alone.
Why Symptom Trend Tracking Matters in Real Clinical Work

1. Therapy Change Is Gradual and Nonlinear
Most clients do not improve in a straight line. Symptoms often fluctuate, intensify, or shift form before stabilizing. Tracking trends over time helps therapists differentiate between:
- Temporary distress during deeper processing
- Meaningful improvement across multiple sessions
- Early warning signs of regression or destabilization
In practice, symptom movement often reflects deeper therapeutic processes rather than surface-level progress. Increased distress may coincide with trauma processing, boundary work, or relational repair — moments that are clinically meaningful but easily misinterpreted when viewed in isolation.
Symptom trend tracking helps therapists contextualize these fluctuations by anchoring individual sessions within a broader arc of care. Rather than reacting to temporary spikes, clinicians can assess whether symptoms are stabilizing, shifting domains, or resolving over time.
2. Clinical Memory Has Limits
Over long treatment histories, even well-documented notes become difficult to synthesize mentally. Therapists are often left scanning old sessions to reconstruct symptom trajectories before reviews, supervision, or care transitions.
When symptom changes are tracked longitudinally, the cognitive burden shifts from recall to interpretation, allowing therapists to focus on meaning, pacing, and next steps rather than reconstruction.
This is especially valuable in:
- Trauma work
- Mood and anxiety disorders
- Chronic or comorbid presentations
- Long-term relational or attachment-focused therapy
3. Documentation Must Demonstrate Medical Necessity
From a documentation standpoint, reviewers are less interested in therapeutic intent and more concerned with observable clinical indicators. Symptom trend tracking creates a defensible link between session content and ongoing need for treatment by showing how symptoms persist, improve, or fluctuate in response to care, supporting:
- Ongoing medical necessity
- Continuity of care
- Clear rationale for continued treatment
Importantly, this can be achieved without introducing rigid outcome measures that disrupt therapeutic flow or over-quantify complex clinical realities.
What Symptoms Are Appropriate to Track?
Effective symptom trend tracking focuses on clinically salient indicators that already appear in your documentation.
| Symptom Domain | Examples of Clinical Symptom Indicators |
|---|---|
| Anxiety | Worry intensity, panic frequency, avoidance |
| Mood | Low mood, anhedonia, energy level |
| Trauma | Hyperarousal, reactivity, intrusive responses |
| Behavioral | Avoidance, impulsivity, withdrawal |
| Somatic | Sleep disturbance, appetite changes |
The goal is not comprehensive symptom capture, but clinical relevance. Symptoms chosen for tracking should reflect the core mechanisms driving distress or impairment, rather than every presenting concern. Over-tracking can obscure meaningful patterns, while focused tracking clarifies symptom progression patterns and treatment impact. In most cases, tracking two to four key symptom indicators is sufficient to reveal symptom reduction trends and guide clinical decision-making.
Common Clinical Pitfalls in Survey-Based Progress Tracking
Many therapy progress tracking tools rely heavily on surveys, rating scales, or check-in questionnaires. While these tools can offer helpful structure, they also introduce limitations that matter in real clinical work.
Treating Survey Scores as the Full Picture
Questionnaire scores can highlight changes in symptom intensity, but they rarely capture why those changes are happening. A score may improve or worsen without reflecting shifts in insight, coping, or relational dynamics discussed in session. When survey data is treated as the full story, important clinical meaning can be missed. Scores are useful reference points but they are not a substitute for clinical interpretation.
Assuming Progress Should Be Linear
Survey-based tools often imply steady improvement from one check-in to the next. In practice, therapy progress is uneven. Symptoms may rise during trauma processing, dip during life stress, or stabilize before improving. When tools are not designed to account for this non-linearity, normal therapeutic fluctuations can be misread as lack of progress or treatment failure.
Losing the Session Narrative
Surveys capture responses about therapy, not the therapy itself. They don’t reflect how themes unfold in conversation, how interventions land, or how the therapeutic relationship evolves. Without grounding trends in session notes, progress tracking risks becoming detached from the clinical work. Narrative context remains essential for understanding what symptom changes actually mean.
From Notes to Trends: How Symptom Monitoring Actually Works
| Step | What Happens Clinically |
|---|---|
| Session documented | Symptoms noted naturally in progress notes |
| Clinical judgment applied | Frequency and intensity reflect therapist assessment |
| Data accumulates | Each session adds a reference point |
| Trends form | Patterns become visible across time |
| Interpretation | Therapist evaluates meaning in context |
In real-world practice, therapy symptom monitoring is rarely linear or perfectly standardized. Language shifts, symptom expressions evolve, and clinical priorities change over time. Effective symptom trend tracking accommodates this reality by allowing patterns to emerge gradually from consistent documentation, rather than forcing strict labels or scoring systems. This approach respects clinical judgment while still enabling longitudinal symptom analysis that supports clarity and continuity.
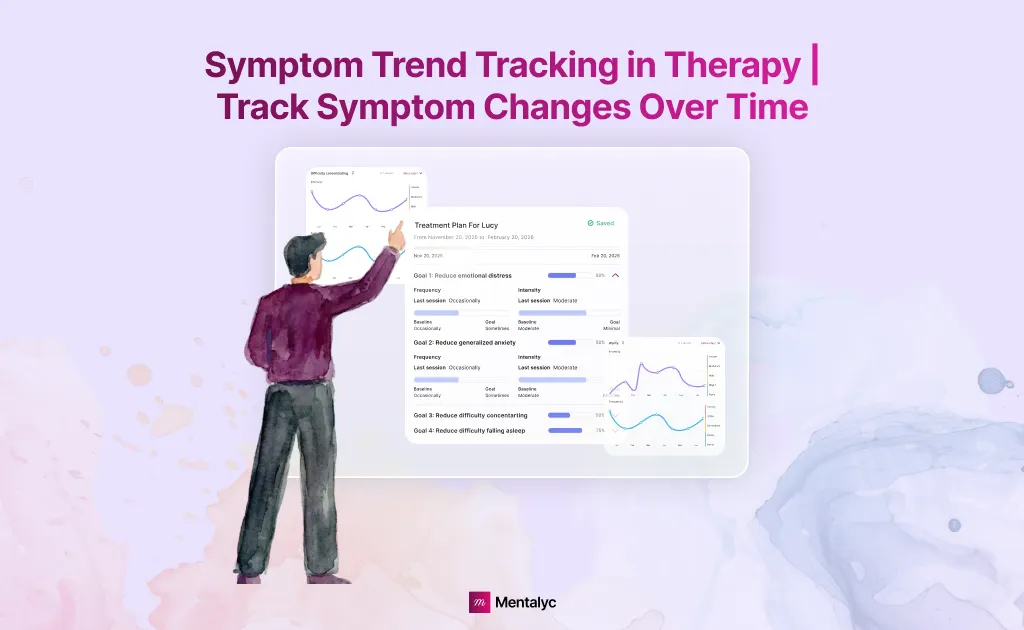
How Mentalyc Supports Symptom Trend Tracking in Therapy
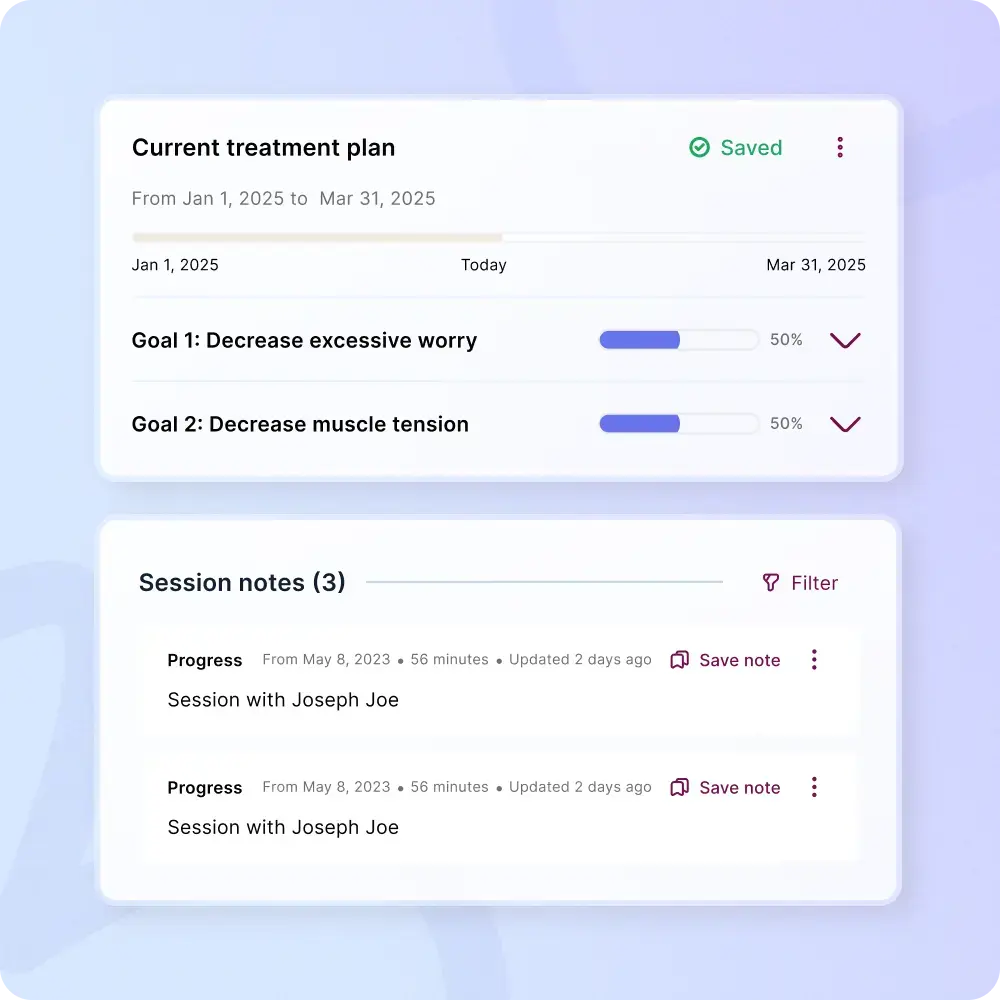
Many symptom tracking tools separate clinical work from documentation by requiring additional forms, client-completed trackers, or post-session data entry. Mentalyc takes a different approach by deriving symptom trends directly from session documentation, keeping the session itself as the primary clinical data source.
Mentalyc’s AI Progress Tracker is designed to help therapists track symptom changes over time using the work they already do—without adding administrative burden.
Here’s how Mentalyc supports symptom trend tracking:
| Stage | What Mentalyc Does |
|---|---|
| Session capture | Upload, record, dictate, or type a session |
| Pattern detection | Identifies key symptoms and themes |
| Ongoing monitoring | Follows symptom frequency and intensity across sessions |
| Visualization | Displays clear symptom trends over time |
| Clinical control | Therapist interprets and decides what matters |
1. Symptom Trends Derived Directly From Session Notes
Mentalyc identifies clinically relevant symptoms from your intake and progress notes and follows them over time. There are:
- No questionnaires
- No client surveys
- No duplicate documentation
The data comes from the session itself.
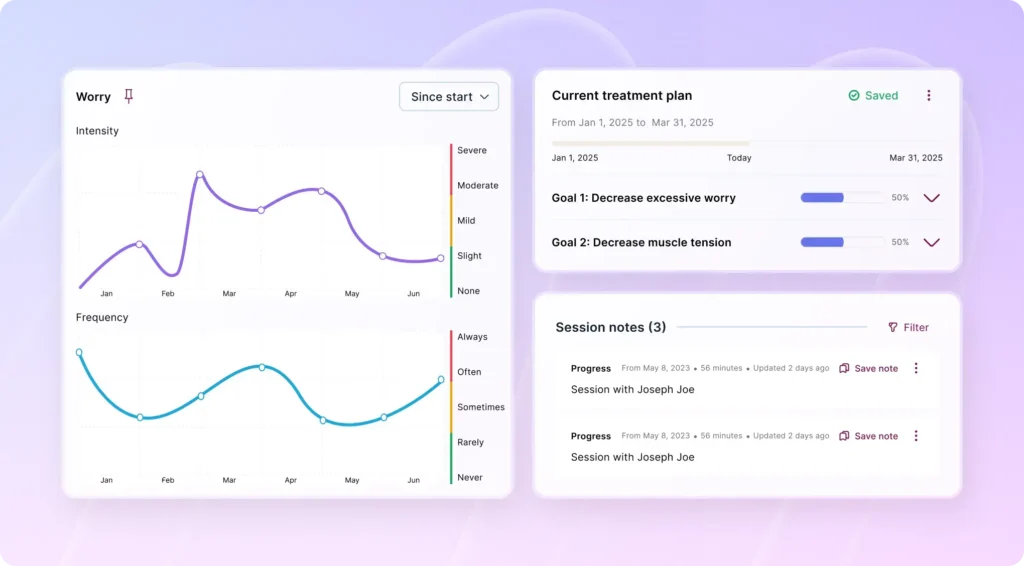
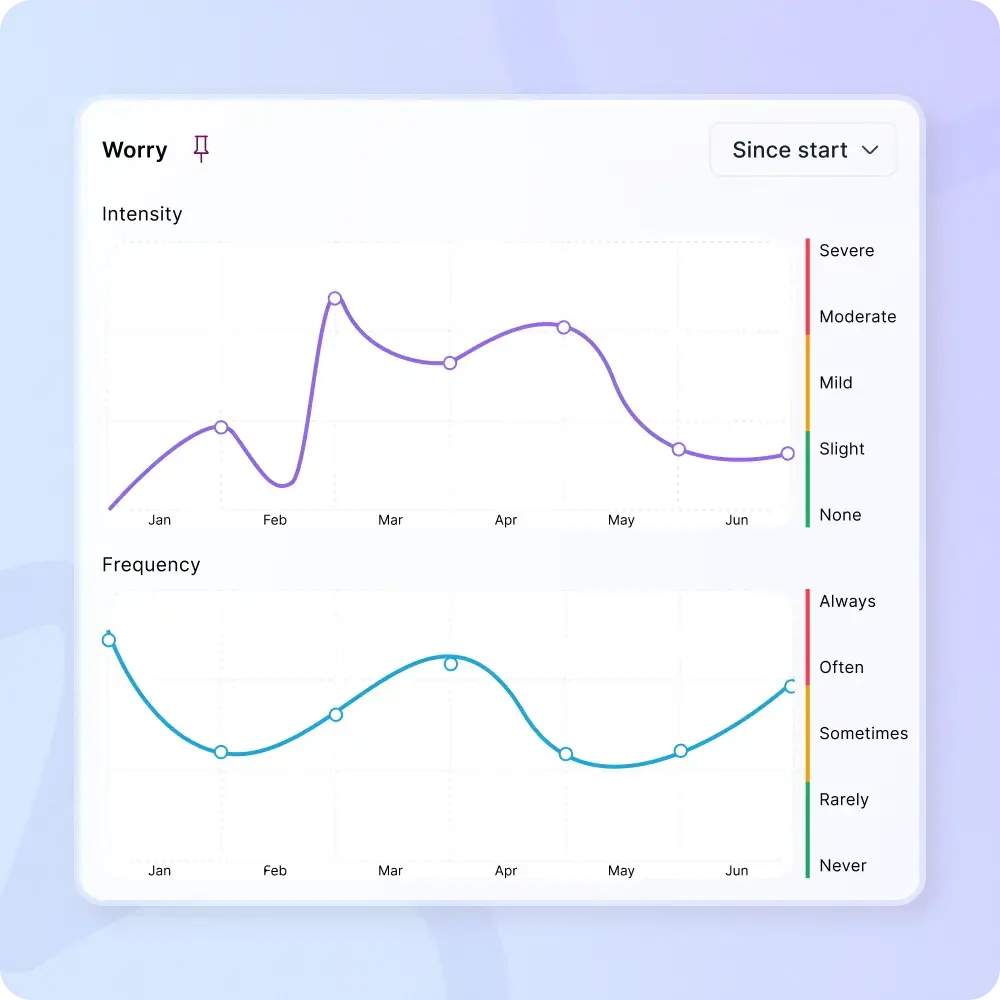
2. Frequency and Intensity Tracking That Reflects Clinical Judgment
Rather than imposing rigid scoring systems, Mentalyc uses the frequency and intensity values already present in your notes. You remain in control of what is tracked and how it is interpreted.
3. Longitudinal Symptom Analysis Without Goal Pressure
Mentalyc’s symptom tracking emphasizes change over time, not outcome targets. This makes it especially useful for therapists who want clarity without heavy goal language or performance framing.
4. Visual Clarity for Complex Cases
Clear charts help therapists:
- See symptom reduction trends
- Identify symptom progression patterns
- Maintain continuity across long treatment histories
- Prepare confidently for reviews or consultations
All without rereading months of documentation.
5. Golden Thread Continuity
Mentalyc connects notes, symptoms, and progress into a single clinical narrative. This continuity supports ethical documentation, clearer clinical reasoning, and stronger confidence in decision-making.
Why Symptom Trend Tracking Strengthens Therapy
When used thoughtfully, symptom trend tracking:
- Supports clear therapy symptom monitoring
- Makes clinical symptom indicators visible over time
- Reduces reliance on memory alone
- Improves confidence in clinical decision-making
- Enhances documentation clarity without reducing nuance
It adds structure without turning therapy into performance metrics.
Conclusion
Symptom trend tracking in therapy is about seeing change clearly over time – not forcing progress into numbers or expecting steady improvement. By looking at symptom frequency and intensity across sessions, therapists can better understand patterns, fluctuations, and meaningful shifts that are hard to track from memory alone.
This approach supports clearer clinical decisions and stronger documentation without disrupting the therapeutic process. It helps show continuity of care and medical necessity while preserving narrative context and professional judgment, especially in long-term or trauma-informed work. Hence, Mentalyc’s AI Progress Tracker supports this by turning session documentation into a clear, longitudinal view of change, without adding forms or separate tracking systems.
Frequently Asked Questions (FAQs) on Symptom Trend Tracking in Therapy
1. What is symptom trend tracking in therapy, and how is it different from traditional progress notes?
Symptom trend tracking in therapy focuses on identifying patterns in symptoms across multiple sessions rather than reviewing each note in isolation. While progress notes document what happened in a session, symptom trend tracking helps therapists track symptom changes over time, revealing broader patterns such as improvement, stability, or escalation through longitudinal symptom analysis.
2. How does therapy symptom monitoring support clinical decision-making?
Therapy symptom monitoring helps therapists observe clinical symptom indicators—such as anxiety severity, sleep disruption, or avoidance—across sessions. By seeing how these indicators evolve, clinicians can make more informed decisions about pacing, focus, or clinical approach without relying solely on memory or single-session impressions.
3. What does symptom frequency and intensity tracking actually measure?
Symptom frequency and intensity tracking reflects how often a symptom occurs and how strongly it is experienced or expressed. Monitoring these two dimensions allows therapists to notice symptom severity changes over time and identify whether shifts reflect temporary fluctuations or meaningful clinical change.
4. Can symptom trend tracking show real therapy-driven improvement?
Yes. When symptoms are monitored consistently across sessions, therapists can observe therapy driven symptom improvement as gradual changes in intensity, frequency, or overall presentation. These symptom reduction trends provide evidence of progress while still honoring the nonlinear nature of therapeutic work.
5. How does Mentalyc help therapists track symptom changes over time?
Mentalyc supports symptom trend tracking by analyzing session notes and identifying symptom patterns automatically. It enables therapists to track symptom changes over time—including frequency and intensity—without questionnaires, surveys, or manual scoring, keeping therapy symptom monitoring grounded in real session data.
6. Are symptom trends meant to replace clinical judgment?
No. Symptom trends are clinical signals, not conclusions. They highlight patterns such as symptom severity changes or stabilization, but interpretation always remains with the therapist. Symptom trend tracking is designed to support clinical judgment, not replace reflective thinking or supervision.
Why other mental health professionals love Mentalyc

“I benefit tremendously every time I wrap up a session and then a few minutes later, I have this AI note. It makes me a better clinician in a variety of ways.”
LPC

“It improves the quality of my work as I review my sessions … I bring a sense of continuity from session to session because of the really good summary and progress notes that Mentalyc gives me.”
Licensed Marriage and Family Therapist

“It helps align the note and the plan for moving forward with sessions … it’s been a really good aid in giving me direction.”
LPC

“I go back and can read the notes, and it really helps me for the next session. It has made me a much better counselor.”
Licensed Professional Counselor