Standardized screening tools like the PHQ-9 and GAD-7 have become routine in mental health care. They are familiar, easy to score, and widely accepted by insurers and healthcare systems. But many therapists are now asking a deeper question: Are self-report questionnaires the best or is it the only way to understand client progress?
This article explores PHQ-9 alternatives for therapists, reviews common GAD-7 alternatives, and then goes further—examining how clinicians can move toward therapy without questionnaires using session-based, clinician-derived insights.
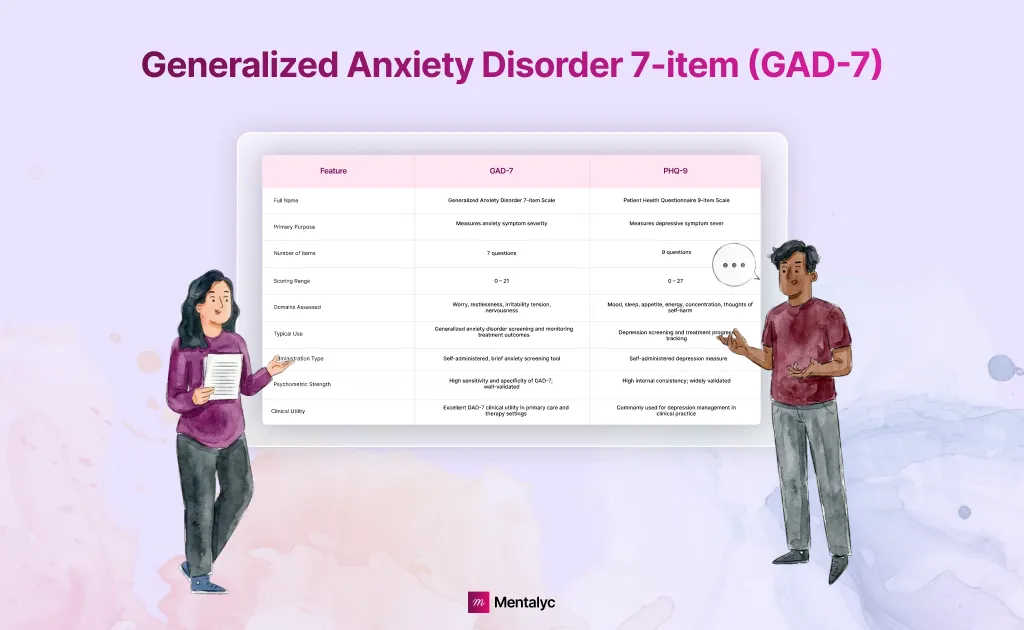
What Are PHQ-9 and GAD-7?
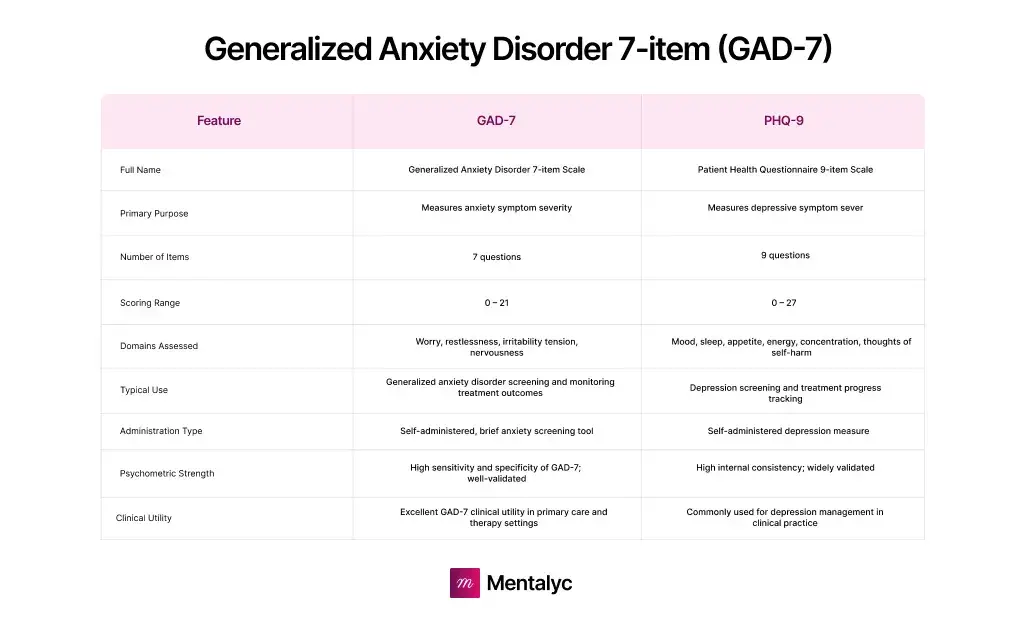
The PHQ-9 (Patient Health Questionnaire–9) is a short questionnaire commonly used to screen for depression and estimate how severe symptoms are. It includes nine questions, each linked to a core depressive symptom such as low mood, sleep problems, fatigue, or trouble concentrating. Clients are asked how often they’ve experienced each symptom over the past two weeks, and their responses are added up to produce a score ranging from minimal to severe depression.
The GAD-7 (Generalized Anxiety Disorder–7) works in much the same way. It includes seven questions focused on common anxiety symptoms like excessive worry, restlessness, irritability, and difficulty relaxing. Clients again reflect on the past two weeks, and their answers are combined into a severity score used for screening or monitoring anxiety.
Both tools were designed to be quick, standardized, and easy to score. They’re especially useful in primary care and settings where clinicians need a fast way to identify symptom severity or decide next steps. What they were not designed to do is capture the lived process of psychotherapy; things like relational change, insight, emotional regulation, or how clients evolve across sessions.
That gap, between measuring symptom severity and understanding therapeutic change, is why many therapists begin to question whether questionnaires alone can truly reflect progress in ongoing therapy.
Common Alternatives for Depression (Alternative to PHQ-9)
| Tool | Primary Use | What It’s Good At | Key Limitations |
|---|---|---|---|
| PHQ-2 | Ultra-brief depression screening | Very quick; useful for initial triage | Only 2 items; lacks depth and nuance |
| PHQ-8 | Depression screening (non-suicide focus) | Similar structure to PHQ-9 without suicide item; often used in research | Removes clinically meaningful risk signal; still self-report based |
| Beck Depression Inventory (BDI-II) | Depression severity assessment | More detailed (21 items); strong research history | Time-intensive; relies entirely on self-report |
| Edinburgh Postnatal Depression Scale (EPDS) | Postpartum depression screening | Tailored to perinatal populations | Narrow population scope; questionnaire-based |
| Geriatric Depression Scale (GDS) | Depression screening in older adults | Designed for age-related factors | Still symptom-focused; limited insight into therapeutic change |
Common Alternatives for Anxiety (Alternative to GAD-7)
| Tool | Primary Use | What It’s Good At | Key Limitations |
|---|---|---|---|
| GAD-2 | Ultra-brief anxiety screening | Fast triage; easy to administer | Only 2 items; minimal clinical depth |
| Beck Anxiety Inventory (BAI) | Anxiety severity assessment | Detailed focus on anxiety symptoms | Over-emphasizes physical symptoms; may inflate severity |
| Overall Anxiety Severity and Impairment Scale (OASIS) | Anxiety severity + impairment | Short; highlights functional impact | Snapshot view; limited insight into therapy process |
| Panic Disorder Severity Scale (PDSS) | Panic disorder assessment | Strong disorder-specific detail | Not suitable for generalized or mixed anxiety |
| HADS / K10 / K6 / ReQoL / EQ-5D-5L | General distress or mental health screening | Broad mental health overview | Not anxiety-specific; limited therapy relevance |
Why Therapists Are Questioning PHQ-9 and GAD-7 Reliance
While self-report questionnaires can be useful early in care, many therapists notice that their value often plateaus as therapy progresses. This isn’t because clients stop changing—but because standardized self-report tools were never designed to reflect the full process of psychotherapy. Across tools like PHQ-9, GAD-7, and their alternatives, several structural limitations become more visible over time.
Client Self-Report Has Real Limits
PHQ-9 and GAD-7 scores depend entirely on how clients rate themselves. That rating can shift based on mood, memory, insight, or how safe a client feels being honest in that moment. A client may underreport during a “good week,” overreport during a crisis, or struggle to translate complex internal changes into fixed answer choices.
As a result, changes in scores don’t always reflect actual progress—or lack of it.
Survey Fatigue Affects Long-Term Therapy
In ongoing work, clients often forget to complete forms, rush through them, or disengage from repeated questionnaires altogether. Over time, these tools can start to feel like paperwork rather than support.
When completion becomes inconsistent, therapists are left wondering whether score changes reflect meaningful shifts or simple form avoidance.
Symptom Scores Miss Much of the Work of Therapy
Standardized scales focus on a narrow set of symptoms. But therapy often targets changes that aren’t easily captured by symptom severity alone—such as improved emotional regulation, relational boundaries, insight, or tolerance for distress.
Clients may be doing important work even when symptom scores remain flat.
Questionnaires Sit Outside the Therapy Session
PHQ-9 and GAD-7 are usually completed outside the session, separate from the therapeutic relationship and moment-to-moment clinical work. This makes it harder to connect scores to why change is happening—or what contributed to a shift. Because they’re detached from session content, questionnaires can miss key clinical context.
Why Many Therapists Are Looking Beyond Self-Report Measures
Taken together, these limitations explain why many clinicians are moving beyond traditional self-report progress tracking. Rather than relying on questionnaires completed outside the session, therapists are increasingly drawn to approaches that stay closer to the therapy itself—approaches that reflect real clinical work and support professional judgment instead of replacing it.
Instead of asking clients to summarize change after the fact, these models look directly at what unfolds across sessions, where therapeutic change actually happens. Progress becomes visible through session-based clinical insights, observable patterns in language and behavior, and themes that emerge over time through interaction—not just through numerical scores.
This way of tracking progress recognizes an important reality: therapy already contains rich, continuous data. The challenge isn’t collecting more information—it’s making the information already present in sessions easier to see, reflect on, and use clinically.
How Mentalyc Enables Progress Tracking Without Surveys
Mentalyc was built around a simple but clinically important insight: the therapy session already contains the richest data about client progress. Questionnaires attempt to approximate change after the fact, but Mentalyc works directly with what unfolds inside the session—language, themes, goals, and clinical movement over time.
This is not a replacement for clinical judgment. Mentalyc is designed to amplify clinician-derived insights, not override them.
Progress From the Session Itself
Most progress-tracking tools start with forms. Mentalyc starts with clinical work. Instead of relying on PHQ-9, GAD-7, or any other self-report scale, Mentalyc’s AI Progress Tracker analyzes anonymized session transcripts generated by the AI Note Taker. From this, it identifies:
- Symptom-related language patterns discussed in session
- Shifts in intensity, frequency, or impact as reflected in clinical dialogue
- Goal-related moments that show movement, stagnation, or change
This allows for survey-free therapy progress tracking that stays grounded in real therapeutic interaction. Because Mentalyc works session by session, progress tracking becomes:
- Longitudinal, not episodic
- Context-aware, not decontextualized
- Clinically interpretable, not just numerical
This approach avoids many well-known client self-reporting limitations, such as mood-dependent scoring, avoidance of questionnaires, or inconsistent completion.
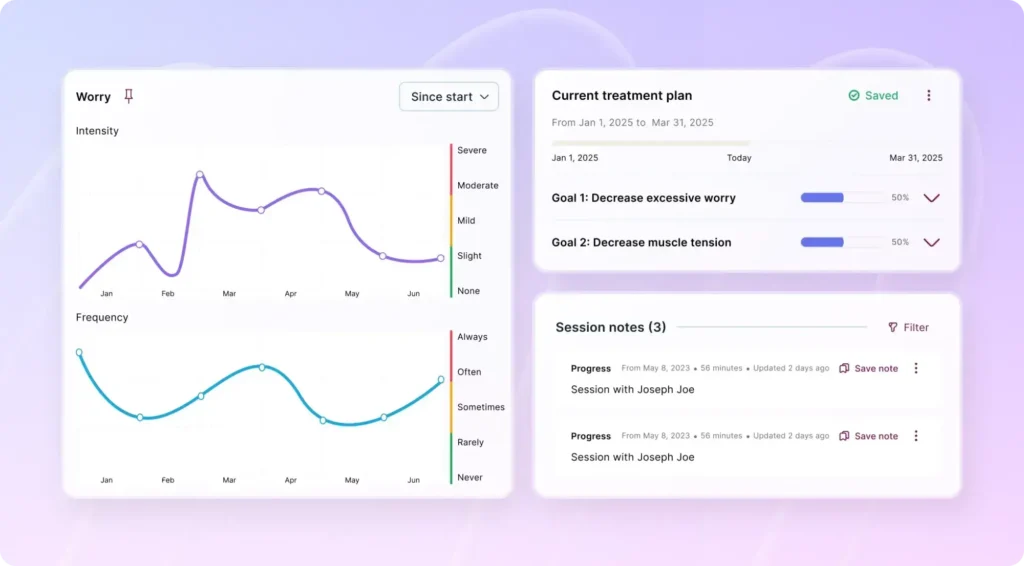
AI Progress Tracker: What It Actually Tracks

Mentalyc does not score symptoms or mimic tools like the PHQ-9 or GAD-7. Instead, the Progress Tracker helps therapists see how change shows up across sessions, using the work that’s already documented.
It focuses on practical, observable patterns such as how client’s presentation reflects changes in symptoms. These are observational clinical data points, extracted from the session itself—not imposed through a checklist.
Progress Without Extra Work
One of Mentalyc’s strongest differentiators is that nothing new needs to be added to your workflow.
- No forms to send
- No surveys to score
- No dashboards to manually update
As long as you document sessions—as you already do—Mentalyc continuously builds a clear, visual picture of progress across time. This is especially valuable for complex, long-term, or nonlinear cases where questionnaires often fail to tell a coherent story.
Goal-Aware Without Relying on Forms
If you use also use treatment plan in Mentalyc, session insights can be linked back to those goals automatically. This makes it easier to see how day-to-day therapy work connects to longer-term treatment direction.
If you don’t use a structured treatment plan, progress tracking still works. Mentalyc looks at patterns in symptoms, themes, and focus across sessions, so continuity is preserved even without goals or questionnaires. In practice, this means:
- You can track progress with or without formal plans or surveys
- Clinical judgment always stays in control
- Subtle, uneven, or nonlinear change is still visible over time
This allows therapists to follow progress in a way that fits real clinical work—without relying on forms, checklists, or rigid scoring systems, while still supporting thoughtful, evidence-informed care.
Ethical, Secure, and Clinician-Controlled
Mentalyc’s survey-free progress tracking is designed to meet real clinical and ethical expectations—not just technical ones.
- Built to meet HIPAA, PHIPA, and SOC 2 requirements
- Session audio is used only to generate transcripts, then removed
- Recordings are not stored long-term
- Client data is not used to train AI models
- Therapists can review, edit, and decide what is kept or used
This approach allows therapists to gain clearer insight into progress without compromising privacy, clinical control, or client trust.
How Mentalyc’s Survey Free Therapy Progress Tracking Works
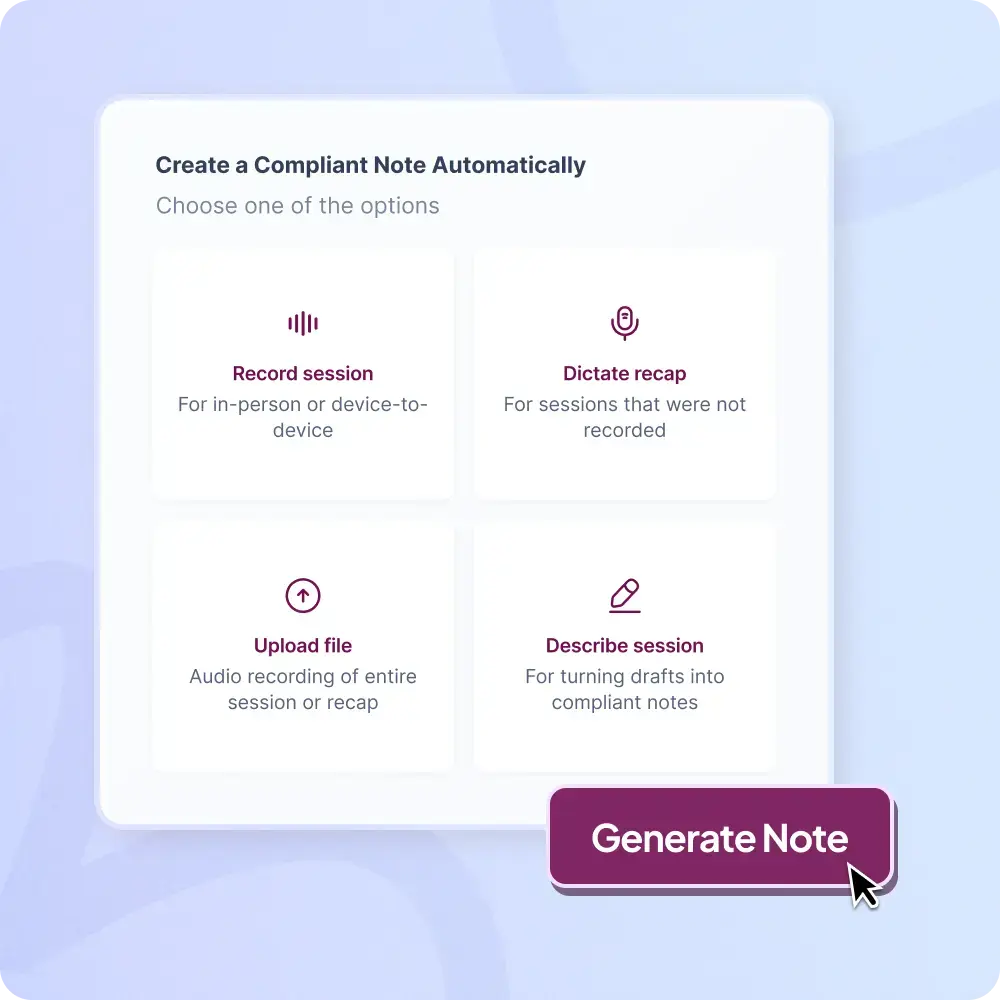
1. Bring your session into Mentalyc
Upload, dictate, type, or record—your usual workflow stays intact.
2. Mentalyc spots what matters
The system identifies key themes, symptoms, and goal-related moments directly from the session.
3. See progress at a glance
Simple visuals reveal trends, shifts, and plateaus across sessions.
Before vs After: Why Clinicians Move Away From Questionnaires
| Before: Questionnaire-Based Tracking | After: Mentalyc’s Survey-Free Progress Tracking |
|---|---|
| Progress relies on PHQ-9, GAD-7, or similar forms | Progress comes directly from therapy sessions |
| Clients forget, avoid, or rush questionnaires | Clients don’t need to fill out anything |
| Scores fluctuate based on mood or context | Patterns emerge across multiple sessions |
| Focus on symptom ratings only | Focus on clinically meaningful change |
| Limited insight into why change happens | Session-based clinical insights show how and why |
| Extra administrative steps for therapists | No added work beyond normal documentation |
| Hard to show continuity in long-term cases | Clear visual story across sessions |
| Clients unsure if therapy is helping | Progress becomes easy to see and discuss |
Conclusion: Moving Beyond Questionnaires Toward Clinically Meaningful Progress Tracking
PHQ-9 and GAD-7—and even their many alternatives—serve an important role in screening and standardized reporting. But they were never designed to capture the full depth of therapeutic change as it unfolds over time. For many clinicians, the growing reliance on surveys has highlighted a fundamental mismatch: therapy is relational, contextual, and nonlinear—while questionnaires are static, reductionist, and external to the session.
Exploring PHQ-9 alternatives for therapists and GAD-7 alternatives is often the first step. Yet for clinicians who want a truer picture of progress, the real shift happens when tracking moves into the session rather than around it.
Mentalyc represents this next step. By enabling survey-free therapy progress tracking grounded in session-based clinical insights, it allows therapists to work beyond self-report measures—without increasing workload or compromising ethics. Progress becomes something you can see, reflect on, and discuss with confidence, all while staying anchored in your clinical judgment.
FAQs: Survey Alternatives, PHQ-9, GAD-7, and Progress Tracking Without Questionnaires
1. What are the best PHQ-9 alternatives for therapists?
Common PHQ-9 alternatives include PHQ-2, PHQ-8, Beck Depression Inventory (BDI-II), Geriatric Depression Scale (GDS), and Edinburgh Postnatal Depression Scale (EPDS). While these tools differ in length or population focus, they still rely on client self-reporting and share similar limitations in capturing session-level therapeutic change.
2. Are there effective GAD-7 alternatives for anxiety tracking?
Yes. GAD-2, Beck Anxiety Inventory (BAI), OASIS, and Panic Disorder Severity Scale (PDSS) are frequently used alternatives. However, like GAD-7, they depend on questionnaires completed outside the session and may miss contextual or relational shifts discussed during therapy.
3. Why do many therapists move toward therapy without questionnaires?
Therapists often move away from questionnaires due to survey fatigue, inconsistent completion, and the limits of self-report data. Questionnaires can miss subtle but clinically important changes, such as improved regulation, insight, or engagement, leading clinicians to prefer session-based, observational approaches.
4. How does survey-free therapy progress tracking work in practice?
Survey-free progress tracking uses session content—language, themes, and goal-related moments—to understand change over time. Instead of scoring forms, clinicians review patterns derived from real sessions, enabling progress tracking that is longitudinal, contextual, and clinically meaningful.
5. Can I track progress without PHQ-9 or GAD-7 and still be evidence-informed?
Yes. Progress tracking does not have to rely exclusively on standardized questionnaires. Using clinician-derived insights, observational clinical data, and session-based patterns can provide a strong, evidence-informed understanding of client progress—especially when viewed across multiple sessions.
6. How does Mentalyc support no questionnaire therapy tracking?
Mentalyc’s AI Progress Tracker analyzes anonymized session transcripts to identify symptom-related patterns, goal movement, and clinically relevant shifts over time. Clients do not need to complete any surveys, and therapists do not need to score or manage forms—progress emerges directly from the session itself.
7. Is progress tracking without surveys suitable for complex or long-term cases?
Yes. In fact, survey-free approaches are often better suited for complex, comorbid, or long-term therapy. By focusing on session-based clinical insights rather than isolated scores, therapists can maintain continuity, recognize nonlinear change, and avoid misinterpreting temporary distress as lack of progress.
Why other mental health professionals love Mentalyc

“I go back and can read the notes, and it really helps me for the next session. It has made me a much better counselor.”
Licensed Professional Counselor

“It helps align the note and the plan for moving forward with sessions … it’s been a really good aid in giving me direction.”
LPC

“It improves the quality of my work as I review my sessions … I bring a sense of continuity from session to session because of the really good summary and progress notes that Mentalyc gives me.”
Licensed Marriage and Family Therapist

“I benefit tremendously every time I wrap up a session and then a few minutes later, I have this AI note. It makes me a better clinician in a variety of ways.”
LPC