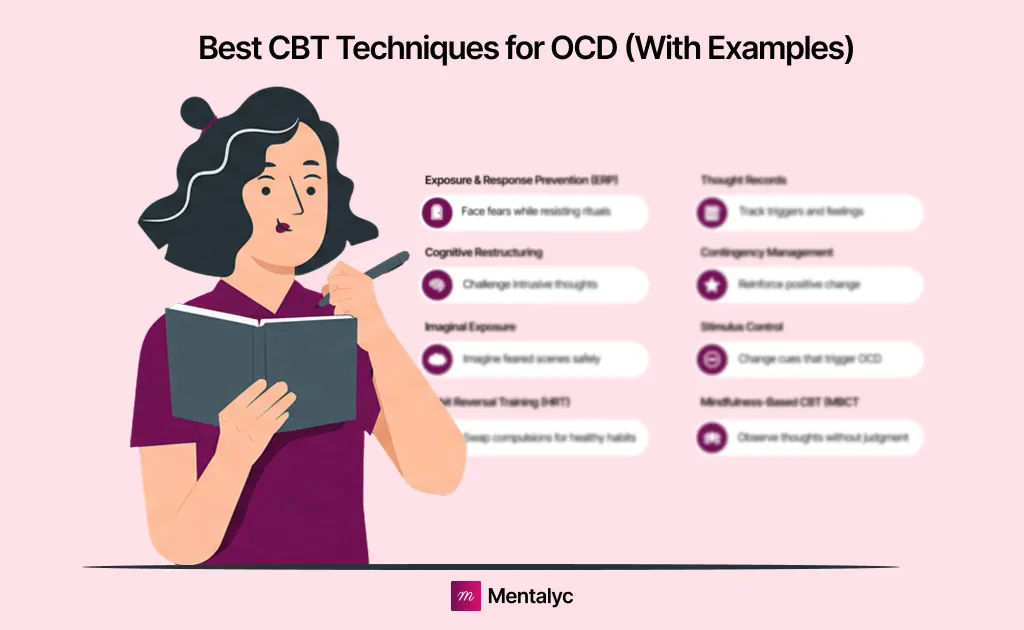
When treating Obsessive-Compulsive Disorder (OCD), therapists often turn to Cognitive Behavioral Therapy (CBT) — the gold-standard approach proven to reduce intrusive thoughts and compulsive behaviors. CBT helps clients recognize and challenge the irrational beliefs that fuel their obsessions while developing healthier coping responses that break the OCD cycle.
In this guide, you’ll explore eight effective CBT techniques for OCD, complete with real-world examples to help you apply them in clinical practice.
As you integrate these techniques into exposure and response prevention (ERP) or other CBT interventions, it’s equally important to monitor how your clients engage with the process. That’s where Mentalyc comes in. Its Alliance Genie™ feature helps you track client engagement and connection throughout ERP work, turning each reflection into measurable therapeutic growth.
What Is CBT and How It Helps With OCD
Cognitive Behavioral Therapy (CBT) is a structured, evidence-based form of psychotherapy that focuses on identifying and changing negative thought patterns and behaviors. It has been widely recognized by the American Psychological Association (APA) and the National Institute of Mental Health (NIMH) as one of the most effective treatments for Obsessive-Compulsive Disorder (OCD).
OCD is characterized by unwanted intrusive thoughts (obsessions) and repetitive behaviors or mental rituals (compulsions) performed to relieve anxiety. CBT helps clients understand the relationship between their thoughts, emotions, and behaviors; ultimately breaking the cycle that maintains OCD symptoms.
Decades of research supported by the APA and NIMH show that CBT, particularly ERP, can significantly reduce OCD symptoms, improve quality of life, and lower relapse rates compared to medication alone. If you want to learn more, check out the CBT cheat sheet.
Advantages and Limitations of CBT for OCD
| Advantages of CBT for OCD | Disadvantages of CBT for OCD |
| Effective in reducing OCD symptoms and related anxiety | Requires significant time, motivation, and client commitment |
| Teaches essential coping and behavioral regulation strategies | May not be suitable for clients with trauma, dementia, or lower intellectual functioning |
| Encourages self-awareness and helps clients recognize thought–behavior patterns | Progress can be slower for individuals resistant to structured or cognitive-based approaches |
Comparison of CBT Techniques vs Other OCD Treatments
| Approach | Main Goal | How It Helps OCD | Key Limitation |
| CBT Techniques (e.g., ERP, Cognitive Restructuring, Mindfulness-Based CBT) | Change unhelpful thoughts and behaviors | Helps clients face fears, reduce compulsions, and develop healthy coping strategies | Requires consistent effort and motivation from clients |
| Medication (SSRIs / Antidepressants) | Reduce OCD symptoms through brain chemistry | Eases intrusive thoughts and anxiety when combined with CBT | May cause side effects; doesn’t address root thought patterns |
| Psychodynamic Therapy | Explore unconscious causes of distress | Increases emotional awareness and insight | Less effective for OCD-specific symptoms; slower progress |
| Acceptance and Commitment Therapy (ACT) | Build acceptance of intrusive thoughts | Helps clients manage distress without fighting their thoughts | Works best when integrated with CBT techniques |
| Mindfulness or Meditation Alone | Promote calm and nonjudgmental awareness | Reduces anxiety and stress linked to obsessions | Helpful as support, not a full treatment |
| Neurosurgical or Brain Stimulation Treatments | Target brain regions involved in OCD | Used only in severe, treatment-resistant cases | Invasive and not widely available |
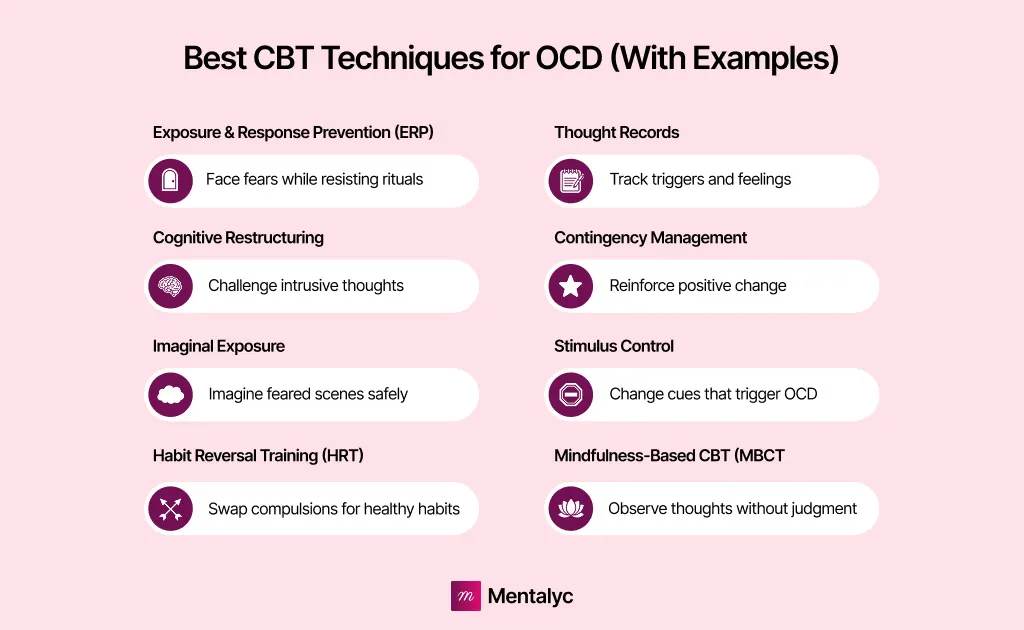
The 8 Best CBT Techniques for OCD (With Examples)
Summary of CBT Techniques for OCD
| CBT Technique | Description | CBT examples for OCD |
| Exposure and Response Prevention (ERP) | Gradual exposure to feared situations or thoughts while preventing compulsive responses. Helps clients tolerate uncertainty and anxiety. | A client with contamination OCD touches a “dirty” object and is guided to resist handwashing until anxiety naturally decreases. |
| Cognitive Restructuring | Identifies and challenges irrational or intrusive thoughts, replacing them with rational, balanced beliefs. | A client who repeatedly checks appliances learns to think, “I verified once, and that’s enough to ensure safety.” |
| Imaginal Exposure | Encourages clients to vividly imagine feared situations that are difficult to reproduce in real life, reducing anxiety through repetition. | A client with intrusive harm-related thoughts imagines the scenario without performing compulsions to neutralize anxiety. |
| Habit Reversal Training (HRT) | Increases awareness of compulsive habits and replaces them with alternative, less disruptive behaviors. | A client who taps their foot eight times before speaking learns to fold their arms instead when the urge arises. |
| Thought Records | Tracks and analyzes automatic negative thoughts (ANTs) to uncover and reframe distorted thinking patterns. | A client who fears losing their job over minor mistakes learns to challenge and reframe the thought based on real evidence. |
| Contingency Management | Uses positive reinforcement to reward clients for resisting compulsions and adopting adaptive behaviors. | A therapist implements a point-based reward system for each successful avoidance of a compulsion. |
| Stimulus Control | Modifies the environment to reduce exposure to OCD triggers, then gradually reintroduces them to build tolerance. | A client initially avoids triggering environments, then progressively re-engages under guided therapeutic exposure. |
| Mindfulness-Based CBT (MBCT) | Combines mindfulness practices with CBT principles to promote nonjudgmental awareness and acceptance of intrusive thoughts. | A client practices observing obsessive thoughts without reacting or engaging in compulsive behaviors. |
Exposure and Response Prevention (ERP) for OCD
Exposure and Response Prevention is an evidence-based CBT technique for managing OCD. It involves the gradual exposure of clients to situations, objects, or thoughts that trigger obsessions. This is conducted in a controlled environment where the client learns to tolerate uncertainty rather than rationalizing their fears.
ERP also assists in preventing clients from engaging in compulsions (rituals). The approach encourages clients to face their fears and realize that the feared outcomes rarely occur. Over time, this reduces anxiety and lessens the severity of obsessions – leading to OCD recovery.
For example, Bridget, who has Contamination OCD, is exposed to touching a “dirty” object. She is then prevented from washing her hands. Gradually, the anxiety linked to not washing decreases. This helps her realize that no negative consequences result from refraining from her compulsion.
**Cognitive Restructuring for OCD**
This entails identifying, challenging, and altering irrational and intrusive thoughts. The cognitive restructuring technique places significant emphasis on modifying these thoughts. Mental health professionals collaborate with clients with OCD to cultivate a well-adjusted and accurate perspective of reality. It also helps them manage their obsessions and reduce the severity or frequency of their anxiety.
For example, Jane tries to leave the house for an urgent outdoor business meeting. However, she keeps going back to check if the light switch in the bedroom is off. This cycle of checking and bolting the door of the room is repeated 10 times within an hour. As a result, she misses the meeting because she cannot leave the house. When asked why she didn’t attend, she explains, “If I don’t check the light switch in my bedroom, my house will burn to the ground.”
Through cognitive restructuring, the therapist helps the client develop rational thoughts. The client learns to think that, “I checked all the appliances once, and that is enough to ensure safety”.
Imaginal Exposure for OCD
This CBT technique for OCD is beneficial for managing obsessions that are often challenging to face. It requires clients with OCD to visualize the feared situation that is difficult or impossible to recreate in real life. The client learns to confront these fears without engaging in compulsive behaviors. This technique teaches the client to tolerate and reduce the associated anxiety over time.
For instance, Gregory struggles with OCD, which causes him to experience intrusive thoughts about harming his colleagues, whenever he receives negative feedback at work. These thoughts are highly distressing for him. He fears losing control even though he would never act on those thoughts. Through imaginal exposure, Gregory learns to face these thoughts and manage his anxiety without performing compulsive behaviors to neutralize them.
Habit Reversal Training for OCD
This CBT technique focuses on pinpointing specific unwanted behaviors linked to OCD. These can include nail-biting, head-scratching, nose-picking, and hair-twirling. The process begins with awareness training. In this case, the clients learn to recognize the urge to engage in these behaviors. Then, these problematic behaviors are replaced with competing responses, which are alternative, and less disruptive actions. HRT is beneficial for clients whose compulsions are not time-consuming but significantly affect their daily lives.
For example, Tommy has a habit of tapping his feet eight times before he answers a question. Through HRT, he first becomes aware of the urge to tap his feet and then learns to substitute this behavior with a less conspicuous alternative. This could be folding his arms in front of him whenever he feels the urge to tap his feet. Over time, this helps him rely less on compulsive behavior.
Thought Records for OCD
Thought records are tools used in CBT to track automatic negative thoughts (ANTs). It is also used to analyze how these thoughts contribute to OCD symptoms. By writing down these thoughts, clients can evaluate the evidence for and against them. This technique gently challenges negative thinking patterns. It helps clients recognize the patterns of their OCD while developing healthier thinking styles.
For instance, Hilary might note the thought: “I’m going to get fired if I don’t do the project presentation perfectly.” The therapist would then assist her in listing the evidence that supports this belief and the evidence against it. She might reframe her thought to: “I’ve made mistakes before, but my boss has never indicated that my presentation style is a problem.” This process helps her challenge and reframe her obsessions.
Contingency Management for OCD
This technique promotes positive behaviors by rewarding clients for abstaining from compulsions. It is a strong motivator for change. Although, the type of reinforcement may differ from one individual to another.
For example, a mental health therapist can work with a client to create a reward system. Here, the client can earn points or privileges each time they resist a compulsion. These rewards act as positive reinforcement when they succeed at hitting their set goal. It also motivates further change.
Stimulus Control for OCD
This approach focuses on changing the environment to reduce exposure to triggers for obsessive-compulsive thoughts (OCT)
For example, a client with OCD might avoid certain people, spaces or objects that trigger their obsessions. Initially, stimulus control involves limiting exposure to these triggers. Later, the therapist gradually reintroduces it during therapy to help build tolerance.
Mindfulness-based CBT for OCD
Mindfulness helps clients accept their thoughts and feelings without judgment. This approach can reduce the power of obsessions. It is often combined with CBT for OCD. It also teaches clients to cope with uncertainty and discomfort which are common challenges in OCD.
For example, Bridget might practice mindfulness by noticing her obsessive thoughts without reacting to them or trying to push them away. Through this, she learns to accept the thought’s presence, observing its effects without acting on the compulsion.
Final Thoughts: Why CBT Is the Gold Standard for OCD Treatment
Cognitive Behavioral Therapy (CBT) remains one of the most effective, research-backed approaches for managing Obsessive-Compulsive Disorder (OCD). Its structured methods, like exposure, cognitive restructuring, and mindfulness, help clients challenge intrusive thoughts, reduce compulsions, and regain a sense of control over their daily lives.
Delivering great care also means staying connected to how clients engage and grow through that process. With Mentalyc, therapists can document progress clearly while gaining deeper insight into client engagement through **Alliance Genie™** – ****a feature that highlights patterns of connection and participation across sessions. It turns reflection into growth, helping you strengthen the alliance that makes CBT so effective.
FAQs About CBT for OCD
Can CBT Cure OCD?
While CBT may not completely cure OCD, it is an effective treatment that can greatly alleviate symptoms. It can enhance daily functioning as it equips clients with the necessary tools to manage their condition and lead fulfilling lives.
How Effective Is CBT For OCD?
Research shows that CBT can significantly reduce symptoms in individuals with OCD. Success rates may be even higher when combined with medication. ERP is also found to be the most effective CBT technique for OCD.
What is the best CBT technique for OCD?
It can vary case by case but the most common OCD treatment method is Exposure and Response Prevention (ERP). ERP helps clients gradually face their fears and resist performing compulsions. According to the American Psychological Association (APA) and National Institute of Mental Health (NIMH), ERP is considered the gold-standard method for reducing obsessive thoughts and compulsive behaviors.
What are the 4 R’s of OCD?
The 4 R’s of OCD are a self-help strategy used to manage intrusive thoughts: Recognize, Re-label, Re-attribute, and Re-focus. This method teaches individuals to identify obsessive thoughts, label them as part of OCD, attribute them to the disorder—not reality—and shift focus toward healthier actions.
What are the best techniques for OCD?
The best cognitive behavioral therapy for OCD include Exposure and Response Prevention (ERP), Cognitive Restructuring, Mindfulness-Based Cognitive Therapy (MBCT), and Habit Reversal Training (HRT). These CBT-based methods help clients challenge intrusive thoughts, tolerate uncertainty, and replace compulsions with balanced coping behaviors.
What is the hardest type of OCD to treat?
The hardest type of OCD to treat is often Pure Obsessional OCD (Pure O), where compulsions occur mentally rather than physically. Because the rituals are internal such as reassurance seeking or mental checking, they’re harder to identify and address through traditional behavioral techniques.
Is CBT or DBT better for OCD?
CBT is generally more effective for Obsessive-Compulsive Disorder than Dialectical Behavior Therapy (DBT). CBT directly targets obsessive thoughts and compulsions using evidence-based methods like ERP, while DBT focuses on emotional regulation and distress tolerance, making it more suitable for borderline personality disorder or emotion dysregulation.
Why other mental health professionals love Mentalyc

“Do yourself a favor, make your life easier. I found Mentalyc to be one of the best tools that I’ve ever used.”
Licensed Marriage and Family Therapist

“For anyone hesitant: this is a lifesaver. It will change your life, and you have more time to be present with your patients.”
Licensed Clinical Social Worker

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)