Writing SMART goals in therapy is one of the most important and most misunderstood skills in clinical practice. Therapists are often trained to think in broad therapeutic aims (“reduce anxiety,” “improve relationships,” “increase insight”), yet documentation, treatment planning, and insurance review require something much more precise. SMART goals bridge that gap. They translate clinical insight into clear, observable, insurance-compliant treatment plan objectives—without losing therapeutic meaning.
This article focuses on how to formulate SMART goals that are clinically sound, ethically appropriate, and usable in real therapy with clinical examples.
What Are SMART Goals in Therapy?
SMART goals in therapy apply the Specific, Measurable, Achievable, Relevant, and Time-bound framework to transform vague aims—such as “feeling less anxious”—into concrete, actionable objectives. By defining precise actions (for example, practicing deep breathing for five minutes during workplace anxiety), these goals create a clear roadmap for therapeutic progress, support client motivation, and keep treatment focused on meaningful outcomes like improved emotional regulation and greater self-awareness.
Components of SMART Goals in Therapy
| SMART Component | What It Means Clinically | Poorly Defined Goal | Well-Defined Clinical Goal | Clinical Notes |
|---|---|---|---|---|
| Specific | Clearly defines what is changing, where, and under what conditions. Avoids vague emotional language. | “Client will feel less anxious.” | “Client will use grounding techniques during episodes of work-related anxiety.” | Ask: What behavior or symptom is changing? In what context? Use observable or behavioral language whenever possible. |
| Measurable | Progress can be observed or evidenced without relying solely on questionnaires. | “Improve emotional regulation.” | “Client will use at least one emotion-regulation strategy on 4 out of 7 days per week.” | Measurement can include frequency, duration, intensity, occurrence/non-occurrence, or therapist-observed functional change. |
| Attainable | Clinically realistic within the current phase of treatment and client capacity. | “Client will eliminate panic attacks entirely within two weeks.” | “Client will reduce panic attacks from 5 per week to 2 per week.” | Consider symptom severity, stage of change, comorbidities, environmental stressors, and available supports. |
| Relevant | Directly connected to diagnosis, functional impairment, and the client’s stated priorities. | “Improve self-confidence” (no clinical link). | “Increase assertive communication in social settings related to social anxiety symptoms.” | For insurance and clinical clarity, goals must link to symptoms and impairment—not just personal growth. |
| Time-Bound | Includes a clear review window for reassessment or adjustment. | “Client will practice journaling regularly.” | “Client will journal at least 3 times per week for the next 30 days.” | Timeframes support structured review, treatment planning, and documentation continuity. |
Common Mistakes Therapists Make With SMART Goals
- Confusing goals with interventions: Goals describe the desired client change; interventions describe what the therapist does to support that change.
- Overloading a single goal: Each goal should track one primary outcome, not multiple behaviors or symptoms at once.
- Using vague language: Terms like improve, increase, or reduce must be clearly defined with observable criteria.
- Omitting review timelines: Without a timeframe, goals cannot be meaningfully evaluated or updated.
- Writing goals only for documentation: Goals should actively guide treatment direction, not exist solely to satisfy paperwork or audits.
Step-by-Step: How to Write a SMART Therapy Goal
Writing a SMART therapy goal is not a single sentence exercise—it’s a clinical reasoning process. Each step builds on the previous one to ensure the goal is therapeutically meaningful, measurable, and defensible in documentation.
Step 1: Identify the Target Issue
Begin by identifying the primary symptom, behavior, or functional impairment that treatment is addressing. This should come directly from assessment data, intake history, and ongoing session content—not from a generalized desire for improvement.
Ask yourself:
- What is the client struggling with right now?
- What is interfering most with daily functioning?
- What symptom or behavior is maintaining distress?
Examples of clear targets:
- Panic attacks occurring at work
- Avoidance of social situations
- Sleep onset difficulties
- Emotional dysregulation during conflict
Avoid framing this step as a value judgment (“low motivation,” “poor coping”). Focus on observable clinical concerns.
Step 2: Make It Specific
Once the issue is identified, define what change would look like in practical terms. This step turns a clinical problem into an actionable direction.
A specific goal answers:
- What will be different?
- What behavior, skill, or symptom expression will change?
- In what context will this change occur?
Examples:
- Instead of “reduce anxiety” → “use grounding techniques during anxiety episodes”
- Instead of “improve communication” → “express needs using ‘I’ statements during conflict”
Specificity prevents goals from becoming abstract aspirations and keeps therapy focused on clinically observable outcomes.
Step 3: Make it Measurable
This is where many therapy goals fall apart. Measurability does not mean over-quantifying—it means defining how progress will be recognized.
Measurement can include:
- Frequency (times per week)
- Duration (minutes or hours)
- Intensity (client-reported scale)
- Consistency (in how many situations the skill is used)
- Reduction or increase in a specific behavior
Examples:
- “3 times per week”
- “for at least 10 minutes”
- “from a 7/10 to a 4/10”
- “in 4 out of 5 situations”
Measurable criteria are essential for treatment plan reviews, progress notes, insurance audits, and clinical decision-making. They allow you to clearly answer the question: Is this goal being met, partially met, or unmet?
Step 4: Evaluate Attainability in the Current Phase of Treatment
A SMART goal must be realistic for the client’s current capacity, not an idealized endpoint.
Consider:
- Symptom severity
- Stage of change
- Cognitive, emotional, or environmental barriers
- Comorbid conditions
- Level of support available
For example:
- Early treatment may focus on skill exposure, not mastery
- Acute distress may require stabilization goals before deeper work
A good clinical check:
“Could this client reasonably work toward this goal over the next few weeks without becoming overwhelmed?”
If the answer is no, scale the goal down—not because expectations are low, but because realistic goals support engagement and success.
Step 5: Ensure Relevance to Diagnosis and Client Priorities
A relevant goal is one that:
- Directly addresses the presenting problem
- Aligns with the diagnosed condition
- Improves functioning or reduces distress
Even well-written goals can fail if they don’t connect to the client’s lived experience.
For example:
- Assertiveness goals may be relevant for social anxiety
- Sleep hygiene goals may be relevant for depression or PTSD
- Emotional awareness goals may be relevant for trauma or relational work
Relevance strengthens the clinical rationale and ensures the goal supports both therapy outcomes and documentation requirements.
Step 6: Define a Clear Timeframe for Review
Every SMART goal must include a time boundary, not to pressure the client, but to structure clinical review.
Timeframes can be:
- Session-based (“over the next 6 sessions”)
- Calendar-based (“within 4 weeks”)
- Phase-based (“by the next treatment plan review”)
The purpose of a timeframe is to:
- Prompt reassessment
- Support clinical decision-making
- Prevent stagnant treatment plans
Without a time component, goals cannot be meaningfully evaluated or updated.
Step 7: Review the Goal as a Whole
Before finalizing the goal, read it as a single statement and ask:
- Is the goal clear without additional explanation?
- Could another clinician understand and evaluate it?
- Does it reflect the client’s real work in therapy?
- Would progress be defensible in an insurance review?
A well-written SMART therapy goal should stand on its own—clinically, ethically, and administratively.
Therapy SMART Goals Examples
These therapy SMART goals examples show how effective goals:
- Focus on behavior and functioning, not just symptoms
- Are measurable without questionnaires
- Match the client’s phase of treatment
- Support clinical decision-making and documentation
Clear goals don’t oversimplify therapy—they make meaningful change easier to recognize, support, and build on over time. Below are examples across common clinical presentations, with a brief explanation of why each goal works in practice.
Anxiety SMART Goals Examples
“Client will practice diaphragmatic breathing for at least 5 minutes during anxiety episodes, 3 times per week, over the next 4 weeks.”
This goal works because it targets a specific coping skill (diaphragmatic breathing), defines when it’s used (during anxiety episodes), and sets a clear frequency and timeframe. It allows both therapist and client to notice whether anxiety is being met with new regulation skills, even if anxiety itself hasn’t fully resolved yet.
Depression SMART Goals Examples
“Client will engage in one planned pleasurable activity per week for the next 6 weeks to improve mood and daily functioning.”
This goal focuses on behavioral activation, a core intervention for depression. It does not require the client to “feel better” immediately. Instead, it measures engagement in life-supporting behavior, which often precedes mood improvement. Progress is observable, achievable, and clinically meaningful.
Social Anxiety SMART Goals Examples
“Client will initiate one brief social interaction per week in a workplace setting for the next month.”
This goal is effective because it defines exposure clearly and gently. It specifies the setting (workplace), the behavior (initiating interaction), and the pace (once per week). It reduces overwhelm while still supporting real-world practice, making progress visible without demanding rapid change.
Trauma SMART Goals Examples
“Client will identify and use one grounding strategy during trauma-related distress in 3 out of 5 occurrences over the next 6 weeks.”
Rather than aiming for trauma resolution too early, this goal prioritizes stabilization and safety. It measures the client’s ability to respond differently during moments of distress, which is often a necessary foundation before deeper trauma processing can occur.
SMART Goals Examples Across Modalities
Many therapists worry that SMART goals feel too behavioral or rigid—especially in approaches that emphasize insight, relationship, or meaning rather than symptom reduction. In practice, SMART goals are theory-agnostic. They do not dictate how therapy is done; they simply provide a clear way to define and review progress. The key is not forcing every modality into the same structure, but adjusting what is measured so it fits the therapeutic approach.
Cognitive Behavioral Therapy (CBT)
CBT aligns naturally with SMART goals because it focuses on observable thoughts, behaviors, and skills. Common CBT goal targets include:
- Skill use (e.g., cognitive restructuring, exposure)
- Behavioral activation
- Symptom frequency or intensity
- Reduction in avoidance
Example: “Client will complete one planned exposure activity per week and record anxiety levels before and after exposure for the next 4 weeks.”
This goal supports CBT principles while remaining specific, measurable, and time-bound.
Dialectical Behavior Therapy (DBT)
In DBT, SMART goals focus on skill application under distress, not eliminating emotions. Goals often track:
- Distress tolerance skill use
- Emotion regulation behaviors
- Reduction in maladaptive coping
- Interpersonal effectiveness practice
Example: “Client will use at least one distress tolerance skill during high-intensity emotional episodes in 3 out of 5 occurrences over the next month.”
This respects DBT’s balance of acceptance and change.
Psychodynamic Therapy
Psychodynamic work centers on insight, patterns, and relational dynamics—areas that can still be tracked without reducing therapy to checklists. SMART goals here focus on observable shifts, such as:
- Increased awareness of recurring patterns
- Changes in relational responses
- Ability to reflect before acting
- Emotional expression in session
Example: “Client will identify and verbalize at least one recurring relational pattern during sessions over the next 6 weeks.”
The goal preserves depth while making progress reviewable.
Humanistic and Person-Centered Therapy
In humanistic approaches, SMART goals are most effective when they are collaborative and client-defined, reinforcing autonomy and self-direction.Measurable elements may include:
- Expressing needs or emotions
- Setting boundaries
- Engaging in values-aligned actions
- Self-advocacy in relationships
Example:
“Client will express a personal need or boundary in at least one interpersonal situation per week for the next month.”
This maintains the spirit of person-centered work while meeting documentation requirements.
Trauma-Focused Therapies (Including EMDR)
In trauma work, SMART goals prioritize stabilization and safety, particularly in early phases of treatment. Goals often track:
- Grounding skill use
- Ability to stay present during triggers
- Reduction in overwhelm or dissociation
- Readiness for trauma processing
Example:
“Client will use a grounding technique during trauma-related distress in 4 out of 6 occurrences over the next 6 weeks.”
This keeps goals clinically appropriate and paced.
Family and Couples Therapy
In relational work, SMART goals focus on interactional patterns, not individual symptoms. Common targets include:
- Communication behaviors
- Conflict-management strategies
- Participation and engagement
- Frequency of escalations or repairs
Example:
“Couple will practice reflective listening during one structured conversation per week for the next 5 weeks.”
This measures system-level change rather than individual pathology.
Writing Treatment Plan Goals That Meet Insurance Expectations
Insurance reviewers are not looking for complex frameworks. They look for consistency.
Specifically, documentation is evaluated for:
- Clear linkage between diagnosis and goals
- Observable indicators of progress
- Time-limited objectives
- Logical alignment between goals, interventions, and progress notes
This alignment—often called the golden thread—connects diagnosis → goals → interventions → progress → review. When that thread is visible, treatment plans are easier to defend. When it breaks, even strong clinical work can appear unclear.
Insurance-compliant goals are therefore less about sophistication and more about precision and continuity over time.
Supporting SMART Goal Formulation Without Extra Work
Formulating SMART goals requires translating real clinical work into language that remains clear across sessions and reviews. In practice, this is where many clinicians experience friction: goals drift from session content, plans become outdated, and documentation starts to feel disconnected from care.
Tools like Mentalyc are useful specifically at this junction—helping keep goals, sessions, and documentation aligned without adding extra work.
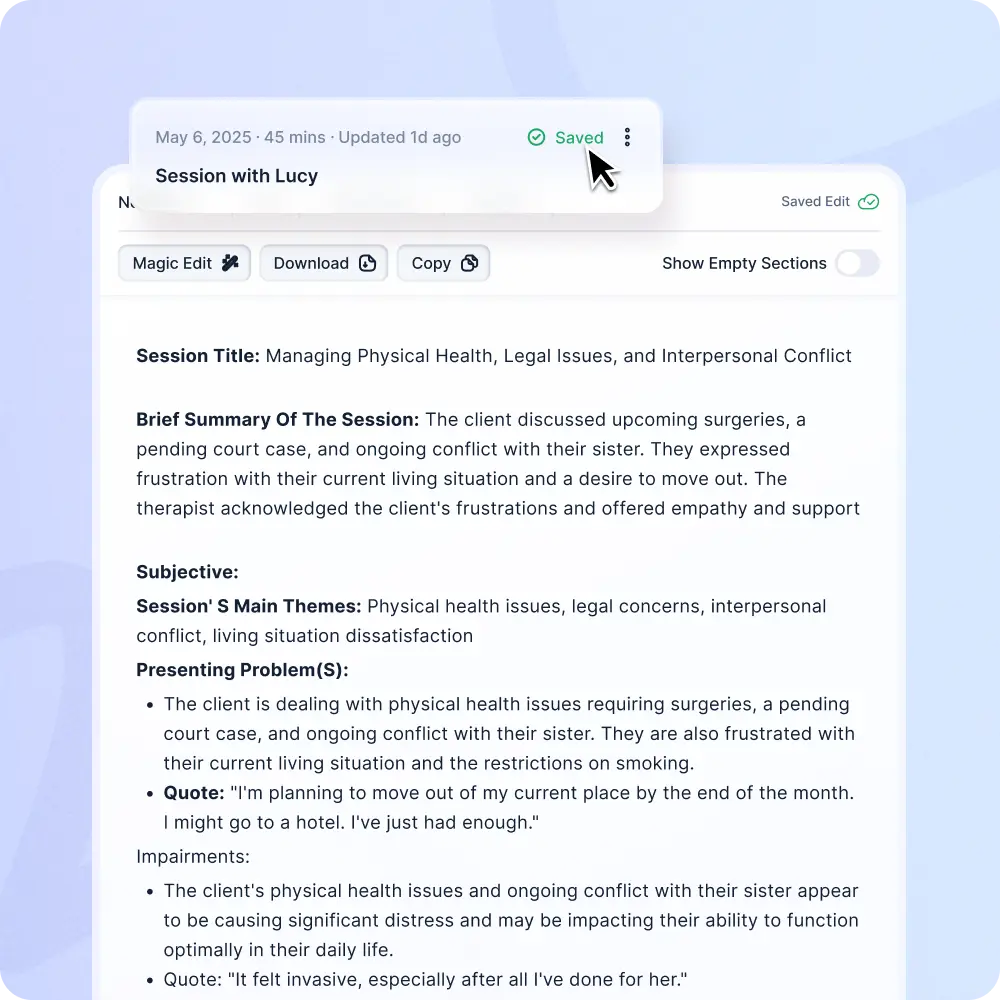
Grounding Goals in Session Content
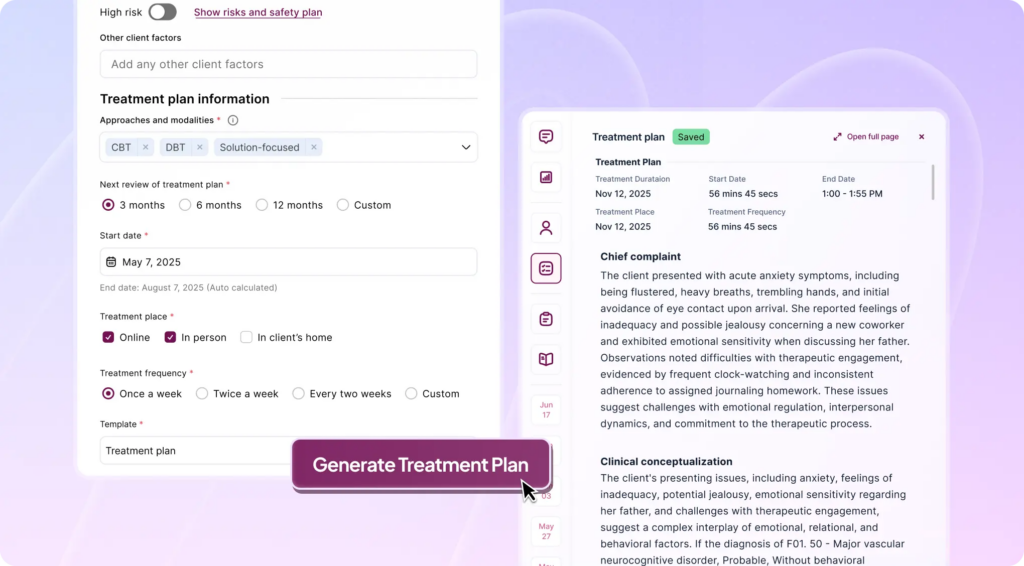
Mentalyc’s AI Treatment Planner works directly from existing session notes to surface clinically relevant patterns such as symptoms, functional impairments, and client priorities. Then, it translates them into SMART-structured goals aligned with diagnosis and treatment rationale. The value here is continuity: goals stay anchored in what actually happens in session rather than being rewritten in abstraction. All suggested goals remain fully editable, preserving clinical judgment and voice.
Maintaining the Golden Thread Over Time
One of the most common documentation issues is goal drift. Initial goals may be well written but lose relevance as treatment evolves. Mentalyc helps reduce this drift by keeping goals connected to diagnosis, interventions, and progress notes. This makes it easier to demonstrate medical necessity and continuity of care during reviews—without adding forms or separate tracking systems.
Keeping Goals Clinically Current
As clients stabilize or gain insight, goals need refinement. Static treatment plans struggle to reflect this reality. As new session notes are added, Mentalyc allows treatment plans to stay current—making it easier to see when goals are being met, adjusted, or replaced, without rewriting entire plans.
Adaptable Across Modalities
SMART goals are not tied to one therapeutic orientation. The Treatment Planner supports CBT, psychodynamic therapy, EMDR, humanistic approaches, and relational work without forcing goals into rigid behavioral language. Clinicians can also customize plan structures to fit their workflow, rather than adapting practice to a fixed template.
Ethical Design and Clinical Control
Any system involved in treatment planning must meet professional and regulatory standards. Mentalyc is built to support this responsibility:
- Fully HIPAA, PHIPA, and SOC 2 Type II compliant
- No session recordings stored
- No client data used for model training
- Clinicians retain full control over all outputs
Technology should support care—not interfere with it.
Conclusion
Writing SMART goals in therapy is more than a documentation exercise. It is a core clinical skill that brings clarity, intention, and direction to treatment. When goals are specific, measurable, attainable, relevant, and time-bound, they transform broad therapeutic aims into meaningful treatment plan objectives that guide interventions, support clinical decision-making, and clearly demonstrate progress over time. Well-formulated SMART goals help therapists stay anchored to observable change while remaining responsive to each client’s unique needs and values.
When supported thoughtfully, SMART goals also reduce documentation strain without compromising clinical depth. Tools like Mentalyc show how session insights can be translated into clear, insurance-ready goals while preserving the therapist’s voice, ethical standards, and theoretical orientation. By keeping goals aligned across sessions and grounded in real clinical work, therapists can spend less time rewriting plans and more time doing what matters most: providing effective, client-centered care.
Frequently Asked Questions About SMART Goals in Therapy
1. What are SMART goals in therapy?
SMART goals in therapy are structured treatment objectives that are Specific, Measurable, Attainable, Relevant, and Time-bound. They help translate clinical insight into clear treatment plan objectives that guide therapy and support insurance-compliant documentation.
2. How are therapy SMART goals different from general therapy goals?
General goals describe broad intentions, while therapy SMART goals examples focus on observable change. SMART goals specify what will change, how progress will be measured, and when the goal will be reviewed—making them clinically actionable and defensible.
3. Do SMART goals require standardized questionnaires to be measurable?
No. Measurable therapy goals can be tracked through observable behaviors, frequency, duration, intensity, or functional change documented in sessions. Questionnaires are optional, not required.
4. How many SMART goals should be included in a treatment plan?
Most treatment plans include 2–5 focused goals, depending on case complexity. Each goal should track one primary area of change to maintain clarity and support effective goal setting in treatment planning.
5. Are SMART goals necessary for insurance documentation?
While not always explicitly required, insurance compliant goals almost always follow SMART principles. Clear, measurable, time-bound goals help demonstrate medical necessity and continuity of care during audits or reviews.
6. Can SMART goals be used across different therapy modalities?
Yes. SMART goals can be adapted to CBT, psychodynamic, trauma-focused, humanistic, couples, and family therapy. The framework structures goals without dictating interventions, supporting flexible clinical goal formulation.
7. How do SMART goals support better treatment planning over time?
By defining specific and measurable objectives, writing treatment plan goals using the SMART framework makes progress easier to evaluate, supports timely goal updates, and keeps therapy aligned with client needs as treatment evolves.
Why other mental health professionals love Mentalyc

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)

“For anyone hesitant: this is a lifesaver. It will change your life, and you have more time to be present with your patients.”
Licensed Clinical Social Worker

“Do yourself a favor, make your life easier. I found Mentalyc to be one of the best tools that I’ve ever used.”
Licensed Marriage and Family Therapist