Mentalyc Blog
-
Therapy practice management software (PMS) assists psychotherapists and counselors in running their practices. The best options combine electronic health records (EHR) and customer relationship management (CRM). In other words, great platforms include client documentation, privacy compliance, and client-focused features and tools. Before therapists sign up for practice management software, they must consider their practice goals and needs. […]
-
In private practice counseling, the first step in getting to know a new client is often through the intake form. This form is like a friendly questionnaire that helps the therapist understand the client's background and what they're seeking help for. A good intake form makes the process smoother and helps the therapist be more […]
-
Are you ready to start an exciting journey as a supervisor for MFT interns? This article is your perfect guide to offering top-notch supervision that helps shape the next generation of therapists and greatly impacts their careers. It covers important topics like handling legal and ethical duties, making sessions meaningful, and trying out new methods. […]
-
Starting your private practice can be both overwhelming and rewarding. While the process requires effort, dedication, and strategic planning on your part, the benefits often far outweigh the challenges. This article explores seven benefits of starting your private practice, providing a detailed look at why you might want to take this professional leap of faith. […]
-
In mental health therapy, creating a supportive environment is important, especially during challenging times. Group therapy is vital in promoting communal healing, allowing individuals to connect with others facing similar struggles. Guided by dedicated professionals, participants find comfort in shared experiences, forming connections that reduce feelings of isolation and stigma. This article offers a practical […]
-
In mental healthcare, understanding the difference between process and content is essential when conducting effective therapy. This article explains what these terms mean and why they matter in different therapeutic settings. Practical examples demonstrate how process and content work in practice. Understanding Content and Process Content and process, while interrelated, serve different purposes, and require […]
-
The treatment plan template by Mentalyc is an excellent tool that can be used by therapists and counselors to map out the path of therapy for their clients. It helps in organizing the goals of the counseling sessions, the methods to be used, and the timeline for achieving these goals. This template serves as a […]
-
Managing a practice involves various administrative tasks that can be time-consuming and complex, but Practice Management Software (PMS) can provide a streamlined solution for handling daily operations. Practice Management Software (PMS) assists in managing daily operations within a clinical practice, including scheduling appointments, billing, managing client records, and ensuring compliance with healthcare regulations. PMS is […]
-
A comprehensive and well-written treatment plan guides therapy sessions by providing structure, focus, and direction. It allows therapists and clients to work together to set goals, tailor interventions, optimize outcomes, and track progress. Treatment plans also facilitate efficient use of session time and promote active client participation. With a roadmap guiding each session, therapists can better prioritize […]
-
Naming your therapy private practice is one of the most meaningful early steps in building your professional identity. It’s more than a creative task; it’s your chance to make a strong first impression, communicate your style, and set the tone for the clients you hope to serve. In this guide, you’ll learn how to choose […]
-
Telemedicine has made it possible to access healthcare services from the comfort of your home, regardless of location or mobility level. The good news is that telepsychiatry enables online counseling, therapy, and medication management, making mental health care more accessible. This guide will provide a detailed overview of telepsychiatry, including its effectiveness, benefits, regulations, applications, […]
-
In therapy, ensuring that you are appropriately compensated for your time and expertise can be a complex challenge. The 8-minute rule is a important but often confusing guideline that forms the foundation of accurate therapy billing. This rule is not just a bureaucratic requirement but essential for ensuring fair payment for your important work. Mastering […]
-
Have you been considering starting a private practice, but not sure how to start? Have you started a private practice and are having difficulty with the billing process? Do you have fears about handling the billing process or not being able to pay someone to handle it for you? Then you have come to the right […]
-
Imagine this: you're wrapping up a counseling session when your client drops a bombshell, something significant that they've been holding back until the very last moment. These revelations are known as 'doorknob confessions,' and they can range from emotional disclosures to discussions of potentially harmful situations. But why do clients often wait until the end […]
-
Have you ever wondered what the ICD-10 code for autism covers? Get ready for an in-depth exploration of this critical tool for mental health professionals. This article delves into the ICD-10 criteria for autism spectrum disorder (ASD), revealing the significance of the F84.0 code. We examine its clinical implications by comparing it with the DSM-5 […]
-
You’ve done it – you leaped private practice! Congratulations! It’s time to get organized and take your practice to the next level. The key to success is having all the essential documents and templates from day one to run your practice smoothly and professionally. In this article, we’ll guide you through the process, from creating […]
-
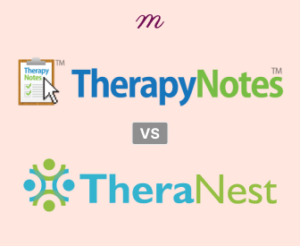
Comparing practice management software options can help mental health professionals seek efficient ways to manage their practices. TheraNest and TherapyNotes are two electronic health records systems that provide excellent value for the mental health practices. TherapyNotes offers straightforward efficiency with its core features. TheraNest, on the other hand, includes Wiley integration and also offers an […]
-
Therapists often seek tools that enhance the effectiveness and efficiency of their practices. Wiley Treatment Planners, a series of resources developed by John Wiley & Sons, Inc., stands out as a valuable tool. Once only available in book format, the treatment planners are now available as online tools on several HER platforms. This article explores […]
-
Evaluating an electronic health record system requires a structured approach considering various factors, from system features to implementation processes and organizational needs. In this blog, you will find a detailed checklist that includes an EHR scorecard, a features checklist, and considerations for assessing the implementation of an EHR system. Why an EHR Needs Assessment? This […]
-
Clinical documents are essential for psychotherapists to maintain organized and confidential records of their clients' treatment and progress. Clear, accurate, and comprehensive documentation supports mental health professionals in providing better care, tracking progress and change, and ensuring compliance with ethical and legal standards. The Vital Role of Clinical Documents in Psychotherapy Clinical documents are truly […]
-
In the US healthcare system, F43.23 is a specific code used for billing within the ICD-10-CM system (effective October 2023). This code signifies a diagnosis of Adjustment Disorder with Mixed Anxiety and Depressed Mood. Remember, international versions of ICD-10 may use different codes for this diagnosis. What does the ICD 10 Code F43.23 stand for? The ICD 10 […]
-
You have patients, right? Or do you have clients? As a therapist, the words you choose hold immense power. They shape the nature of your relationships with those you serve. Whether you use the term “clients” or “patients,” each carries its own weight. This weight can influence the dynamics of your interactions and the effectiveness […]
-
Have you ever been curious about the secrets behind those tricky multiple-choice questions in an assessment? Brace yourself as we take you on an exhilarating journey to the world of psychometric assessments! Psychologists have ingeniously crafted psychometric assessments to measure various traits, abilities, and preferences. By quantifying attributes that are not visible to the naked […]
-
Exploring the Dynamics of Therapeutic Relationships Have you ever pondered the profound impact of the therapeutic relationship on healing? It’s often stated that the bond between the client and the therapist reigns supreme in therapy. While techniques and theories have their place, the human connection truly drives change. This article delves into the art and […]