The Clinician-Administered PTSD Scale (CAPS) is widely recognized as the gold standard for diagnosing and assessing Post-Traumatic Stress Disorder (PTSD). This structured interview helps therapists evaluate how trauma shows up in daily life — from symptom intensity and frequency to real-world impact.
In this guide, we’ll unpack how CAPS works, what makes it so reliable, and how to use the latest CAPS-5 version for more accurate, defensible diagnoses.
If you regularly assess trauma or monitor symptom changes, Mentalyc’s Progress Tracking helps you visualize patterns and improvements across sessions — turning your notes into clear, data-backed insight on client recovery.
Comprehensive PTSD assessment with CAPS
Developed by the U.S. Department of Veterans Affairs National Center for PTSD, CAPS has been refined over time to stay current with the Diagnostic and Statistical Manual of Mental Disorders (DSM). The latest version, CAPS-5, aligns with the DSM-5 criteria, offering clinicians a clear and standardized method for accurate PTSD assessment (Jackson et al., 2024).
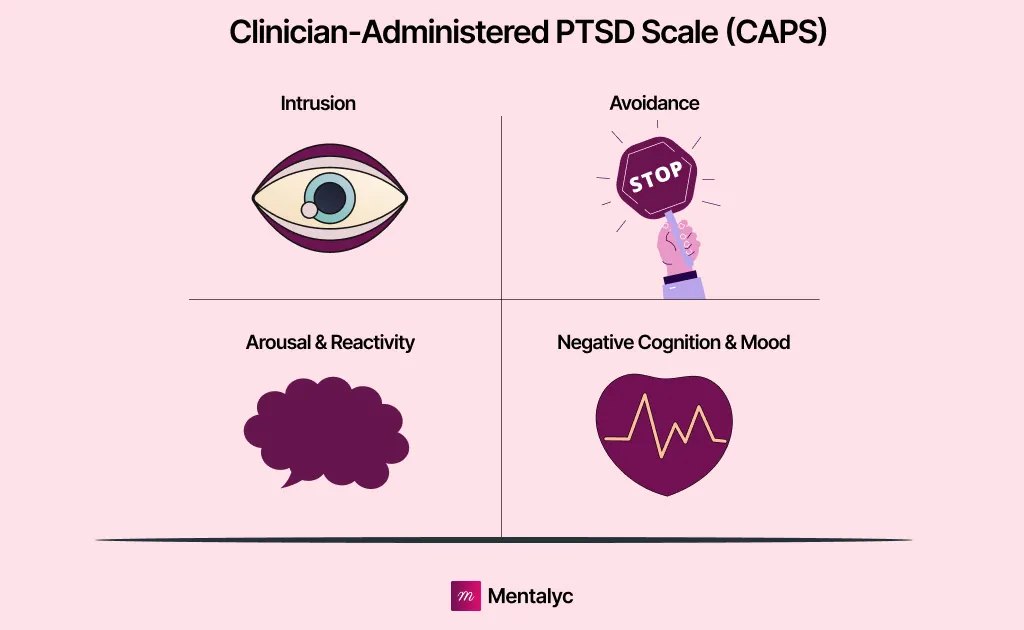
First designed for diagnosing PTSD, the CAPS is a special tool used for appraising the prevalence, frequency, and intensity of symptoms among traumatized individuals. The CAPS, as a gold standard in diagnosing PTSD, ensures that each symptom meets the criteria laid down in intrusiveness, avoidance, negative alteration of mood and cognition, and heightened arousal presented by the DSM-5.
This format communicates to the clinician in a standardized way whether a person either does or does not meet the diagnostic threshold for PTSD. At the same time, measuring symptom severity and functional impairment. Clinically, CAPS for PTSD diagnosis is used to aid in treatment decisions that will assist the mental health professional by monitoring changes in symptoms or assessing the effectiveness of interventions.
It further plays an important role in research, military, and forensic settings by providing reliable data on the prevalence of PTSD, treatment outcomes, and disability claims. CAPS allows the capturing of both qualitative and quantitative aspects of PTSD, hence providing a comprehensive and evidence-based assessment. This makes it an indispensable tool in trauma-related mental health care (Lee et al, 2022).
Structure and Metrics of the Clinician-Administered PTSD Scale
| DSM-5 Symptom Cluster | Description | Example Symptoms | CAPS-5 Assessment Focus |
| Cluster B: Intrusion Symptoms | Recurrent and distressing recollections or re-experiencing of the traumatic event. | Flashbacks, nightmares, intrusive memories. | Frequency and intensity of intrusive experiences. |
| Cluster C: Avoidance | Persistent efforts to avoid trauma-related stimuli. | Avoiding thoughts, conversations, people, or places related to the trauma. | Extent of avoidance behaviors and emotional detachment. |
| Cluster D: Negative Alterations in Cognition and Mood | Persistent negative beliefs, emotions, or detachment resulting from trauma. | Guilt, shame, distorted self-blame, inability to feel positive emotions. | Emotional tone, cognitive distortions, and interpersonal impact. |
| Cluster E: Alterations in Arousal and Reactivity | Heightened physiological and emotional arousal following trauma. | Irritability, hypervigilance, exaggerated startle response, insomnia. | Monitoring of arousal levels and functional impairment. |
The CAPS is a structured interview with a trained clinician and represents the DSM-5 symptom criteria for PTSD, which are categorized into four primary symptom clusters: intrusion symptoms, avoidance, negative alterations in cognition and mood, and alterations in arousal and reactivity. Intrusion symptoms refer to one or more of the following: recurring, distressing recollections; nightmares; flashbacks; or intense psychological distress related to the trauma.
Avoidance refers to efforts to avoid thoughts, feelings, or reminders associated with the trauma. Negative changes in cognition and mood are presented by persistent negative beliefs, emotions, detachment from others, and inability to experience positive emotions. In arousal and reactivity, these include irritability, hypervigilance, exaggerated startle response, and difficulty concentrating or sleeping.
Each symptom is rated in terms of frequency and intensity on a PTSD evaluation scale ranging from 0 (Absent) to 4 (Extreme/Severe). A final diagnosis of PTSD is made by meeting the DSM-5 symptom threshold criteria based on the total CAPS score. CAPS also consists of clinician-rated global severity and impairment measures, thus making it quite a detailed and comprehensive tool (Marx et al, 2022).
Who Uses CAPS?
The majority of the users of CAPS are mental health professionals, researchers, forensic professionals, and clinical trial investigators. It is used by psychologists, psychiatrists, and licensed mental health clinicians in diagnosing PTSD and creating treatment plans for patients.
Researchers into the prevalence of PTSD, treatment effectiveness, or neurological effects of trauma use the CAPS because of its detail in assessment. Clinicians in VA settings, along with forensic experts, apply the CAPS in the assessment of disability and legal cases involving PTSD.
Clinical trial investigators also use the CAPS to establish a baseline of PTSD severity and to monitor changes in symptoms over time. Since the CAPS requires formal training, it is not a self-report tool and should only be administered by professionals familiar with PTSD assessment and criteria for diagnosis according to the DSM.
Benefits of the Clinician-Administered PTSD Scale
These many benefits range from being the gold standard in clinical and research assessments of PTSD. Its most salient feature is that it ensures, comprehensively and in a structured manner, that PTSD symptoms are assessed in detail according to the DSM-5 criteria.
CAPS provides a detailed symptom severity rating so that clinicians are able to show distinctions between mild, moderate, and severe presentations of PTSD. Its high degree of reliability and validity makes this tool very effective for diagnosis, treatment planning, and monitoring of symptom course and progression over a period of time.
Unlike other self-report measures, CAPS incorporates clinician judgment that therefore helps reduce probable biases or inaccuracy arising in the process while patients assess themselves. Further, clinical trials and forensic reviews are added to its usability, as it can monitor the treatment effects, the effectiveness of intervention, and can support legal or disability claims. Since CAPS offers a structured yet flexible interview format, clinicians can tailor their assessments to the individual, which will provide a much more nuanced understanding of PTSD and its impact on daily functioning.
Is CAPS Evidence-Based?
CAPS has, in general, been considered one of the evidence-based PTSD assessment tools. Inter-rater reliability has consistently demonstrated a very strong consistency of the results obtained when different clinicians evaluate the same patient. There is also high convergent validity with the results obtained using the PTSD Checklist, for example. Moreover, predictive validity such that CAPS is able to be used by both clinicians and researchers in predicting PTSD symptom severity and functional impairment into the future.
As one of the measures with very strong reliability and validity, CAPS is usually included in randomized clinical trials to examine treatments for PTSD. Due to its temporal changes in symptom detecting, the role of a gold standard diagnostic measure for the disease is underpinned (Possemato et al, 2023).
How to Administer and Use CAPS
The administration of CAPS requires structured training along with a background of trauma assessment methodologies. The interview typically takes 45–60 minutes to administer, although this can be shorter or longer depending upon symptom severity and patient responsiveness.
The process initiates with the trauma history screen, in which the clinician identifies a single most distressing traumatic event to the patient. All symptoms present within the DSM-5 criteria for PTSD are assessed for their frequency and intensity, and rated by the clinician. A person’s overall score is considered against the criteria of diagnosis for PTSD.
After the CAPS-5 administration and scoring, results are interpreted for diagnosis, research, or treatment planning by a clinician. High scores denote severe symptoms in CAPS and low scores for mild or subclinical PTSD. Trauma assessment tools for clinicians such as CAPS provides a very much-needed insight regarding the course of treatment over some time as fluctuations in the CAPS scores clearly indicate an increase or decrease in symptoms (Rivest-Beauregard et al, 2022).
Limitations of the Clinician-Administered PTSD Scale
Although highly reliable and valid, there are a number of limitations associated with the CAPS. First of all, this is a very time-consuming tool because a complete interview may take nearly an hour; hence, its use in routine clinical screenings is not appropriate. Because the rating on the CAPS requires a trained clinician, it is less accessible compared to self-report measures such as the PTSD Checklist for DSM-5.
Other limitations include the subjective nature in the ratings since symptom scoring depends on the subjective judgment of clinicians, there might be some variance between assessors. Moreover, discussing traumatic life events can also be disturbing to patients and, for the clinician, may require trauma-informed practice-to comfort the patient and ensure retraumatization does not take place (Possemato et al, 2023).
The PTSD clinician rating scale, known as the Clinician-Administered PTSD Scale (CAPS), is a highly structured, evidence-based tool with exceptional reliability and validity for the assessment of symptoms of PTSD. Extensively used in clinical practice, research, and forensic settings, it is considered the gold standard for diagnosing PTSD. However, there are some limitations due to the time-consuming nature and need for trained clinicians to use this scale. Despite such challenges, CAPS remains invaluable in the understanding of the severity and impact of PTSD and the guidance of treatment.
Mentalyc: Smart Documentation Solutions for Mental Health Professionals
Mentalyc is a Clinical Intelligence platform that supports trauma-focused care by automatically capturing symptom trends and progress across sessions without the need for doing manual notes. It can help you connecting what’s said in session to measurable outcomes, keeping documentation accurate, compliant, and clinically meaningful.
By transforming voice or written inputs into clear, compliant documentation, Mentalyc supports clinicians in focusing on what truly matters — providing compassionate, evidence-based care.
Mentalyc Plans & Pricing
| Plan | Price | Key Features |
| 14-Day Free Trial | $0 | 14 days of full PRO access, including 15 notes—no credit card required. |
| Mini | USD 14.99 /month | Record in-person sessions, upload audio files, use voice- to-text, or type notes directly, etc |
| Basic | USD 29.99 /month | Everything in Mini, plus: Alliance Genie™NEW! (limited access), Smart TP™ |
| Pro | USD 59.99 /month | EMDR, Play and Psychiatry modalities, 100+ custom templates incld. BIRP, PIRP, GIRP, PIE, and SIRP, Auto-computed CPT codes |
| Super | USD 99.99 /month | Everything in Pro, plus: Group therapy notes for each group member, Priority onboarding and support |
For more information, visit the pricing page on our website.
Frequently Asked Questions About Clinician-Administered PTSD Scale (CAPS)
1. What is the Clinician-Administered PTSD Scale (CAPS)?
The Clinician-Administered PTSD Scale (CAPS) is a clinician-administered interview for PTSD used to diagnose and assess the severity of post-traumatic stress disorder symptoms. Developed by the U.S. Department of Veterans Affairs National Center for PTSD, it is recognized as the gold standard for PTSD diagnosis. The CAPS PTSD assessment evaluates both the presence and the intensity of trauma-related symptoms, providing a detailed understanding of how these symptoms affect daily functioning. It aligns with the DSM-5 diagnostic criteria for PTSD and is suitable for both clinical and research applications.
2. What Is the Structure and Scoring of the CAPS-5?
The CAPS-5 is a PTSD structured interview that systematically evaluates each of the DSM-5 PTSD symptom clusters — intrusion, avoidance, negative alterations in cognition and mood, and arousal/reactivity. Each symptom is rated for both frequency and intensity, with scores ranging from 0 (Absent) to 4 (Extreme/Severe). This frequency and intensity rating of PTSD symptoms allows clinicians to determine whether a patient meets the diagnostic threshold and to measure symptom severity. The total CAPS score reflects the overall impact of PTSD symptoms on the individual’s daily life.
3. Who Uses the CAPS for PTSD Diagnosis?
The CAPS is primarily used by licensed mental health professionals, such as psychologists, psychiatrists, and trauma specialists. It is also widely applied in PTSD assessment in clinical and research settings, where its precision supports diagnosis, treatment planning, and data collection. Additionally, forensic applications of CAPS include evaluations for disability claims, legal proceedings, and military service-related trauma cases. Researchers rely on the tool to assess the efficacy of interventions and to explore the neurobiological impact of trauma.
4. What Are the Benefits of Using CAPS in Clinical Practice?
The CAPS is a valid and reliable PTSD measure that ensures a comprehensive and standardized assessment of PTSD symptoms. It provides clinicians with a structured diagnostic tool for trauma that integrates clinical judgment with standardized symptom ratings. Using CAPS helps in monitoring treatment outcomes in PTSD, as changes in scores over time indicate symptom improvement or worsening. Its structured nature also promotes diagnostic consistency across clinicians and enhances the quality of treatment planning and evaluation.
5. How to Administer the CAPS-5 Interview?
Administering the CAPS requires adherence to CAPS training and administration guidelines, as it involves a detailed, semi-structured interview format. The assessment typically lasts 45–60 minutes and should be conducted by a trained clinician familiar with trauma evaluation. The process begins with identifying the most distressing traumatic event, followed by exploring each PTSD symptom for frequency and intensity. The clinician rates responses according to the standardized scoring system, ensuring diagnostic accuracy and consistent measurement across sessions.
6. What Are the Limitations and Considerations in Using CAPS?
Although the CAPS is considered the DSM-5 PTSD assessment tool of choice, it has some limitations. It can be time-intensive, requiring both specialized training and clinical experience. The assessment process may also be emotionally demanding for clients, necessitating a trauma-informed approach. Additionally, subjective differences in clinician ratings can introduce some variability. Despite these considerations, CAPS remains one of the most comprehensive and empirically supported PTSD clinical research instruments available.
7. What Is the Purpose of a CAPS Score?
The CAPS score quantifies the severity of PTSD symptoms and determines whether an individual meets diagnostic criteria. It allows clinicians to differentiate between subthreshold, mild, moderate, and severe cases of PTSD. Beyond diagnosis, the score provides valuable data for evaluating treatment effectiveness and tracking symptom progression over time. As such, the CAPS score is an essential component of monitoring treatment outcomes in PTSD and guiding individualized care plans.
8. What Is the Age Range for the Clinician-Administered PTSD Scale?
The standard CAPS-5 is designed for adults aged 18 years and older. However, there are developmentally appropriate versions such as the CAPS-CA-5 (Clinician-Administered PTSD Scale for Children and Adolescents), which is suitable for individuals aged 7 to 17 years. These versions maintain the same diagnostic rigor and standardized format, ensuring consistency across age groups when conducting a PTSD structured interview for diagnostic purposes.
Why other mental health professionals love Mentalyc

“It helps align the note and the plan for moving forward with sessions … it’s been a really good aid in giving me direction.”
LPC

“I go back and can read the notes, and it really helps me for the next session. It has made me a much better counselor.”
Licensed Professional Counselor

“It improves the quality of my work as I review my sessions … I bring a sense of continuity from session to session because of the really good summary and progress notes that Mentalyc gives me.”
Licensed Marriage and Family Therapist

“I benefit tremendously every time I wrap up a session and then a few minutes later, I have this AI note. It makes me a better clinician in a variety of ways.”
LPC