Effective documentation is a cornerstone of quality patient care. Therapy progress notes serve as a vital tool for clinicians to communicate and collaborate with colleagues, ensuring continuity and providing a comprehensive understanding of a patient’s journey.
While progress notes are essential for legal and reimbursement purposes, they also play a crucial role in tracking treatment outcomes and facilitating evidence-based decision-making. To maximize the impact of your care, employing precise and clinically meaningful progress note terminology is essential.
Using clinical words for progress notes that accurately capture a patient’s symptoms, emotions, and behaviors not only improves communication but also contributes to a more nuanced understanding of their condition.
Precise terminology allows for better collaboration among healthcare professionals, reducing the risk of miscommunication and ensuring appropriate treatment interventions.
As such, this blog post will explore a variety of clinical words to use in your progress notes while providing valuable insights on how to enhance your documentation skills.
| Category | Clinical Words / Phrases |
| Mood & Affect | Flat affect, labile, dysthymic, euphoric, anxious, irritable, apathetic |
| Thought Process | Linear, circumstantial, tangential, perseverative, flight of ideas, disorganized |
| Behavior & Activity | Withdrawn, cooperative, guarded, restless, agitated, lethargic, hyperactive |
| Speech & Communication | Pressured, coherent, slurred, monotone, articulate, circumlocutory |
| Cognition & Orientation | Alert, oriented x3, confused, impaired memory, distractible, poor concentration |
| Insight & Judgment | Limited, intact, impaired, poor, fair, good |
| Risk & Safety | Suicidal ideation, self-harm behavior, homicidal thoughts, high-risk, safety maintained |
Feeling Stuck? Here’s How The Right Clinical Words Make Therapy Documentation Easier
I’ll be honest – writing progress notes is one of those tasks I still find challenging. You probably know the feeling: you understand what needs to be documented, but figuring out how to phrase it can be frustrating. That’s where having the right [mental health documentation words] makes all the difference, turning a stressful task into a clear, structured process.
Drawing upon my diverse background of working across various agencies, I humbly acknowledge that I do not possess absolute mastery. However, through diligent effort, I have managed to enhance my proficiency in composing comprehensive notes using psychiatric progress note vocabulary.
Each one of you probably has a distinct approach to documenting patients’ records, yet I have come to appreciate the following methods as my personal favorites for clinical documentation for therapists.
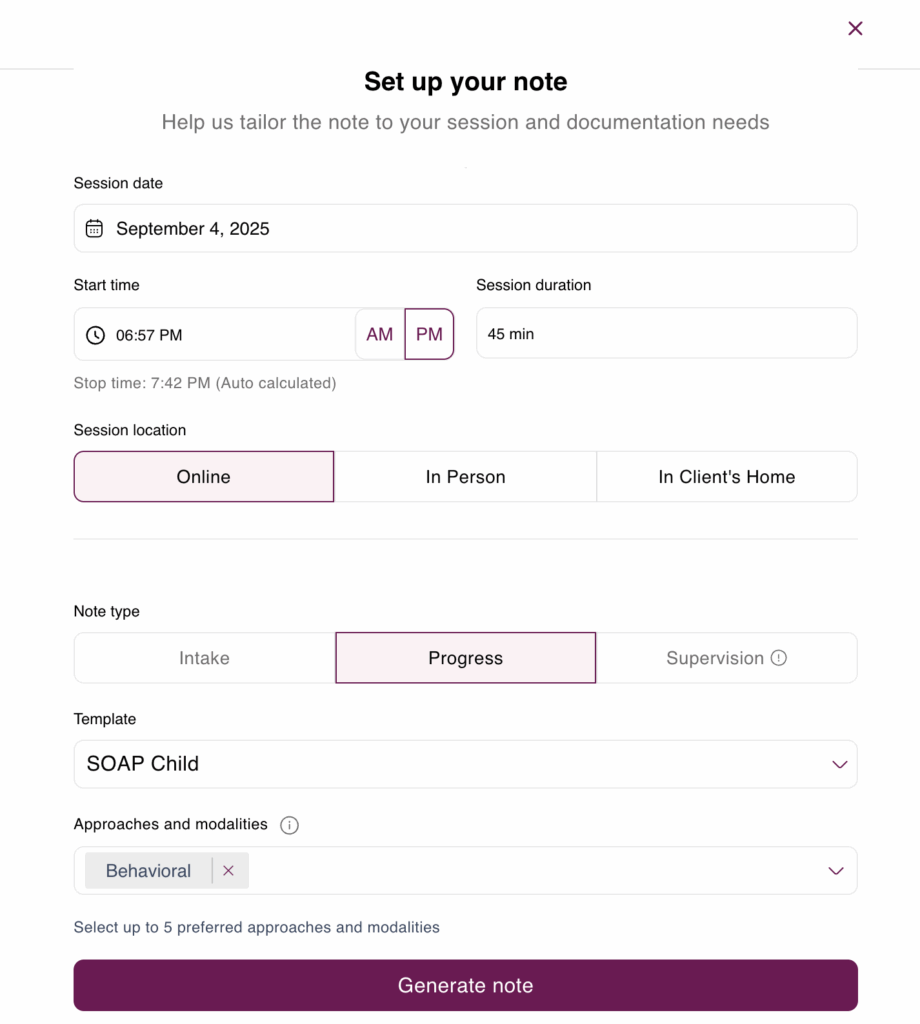
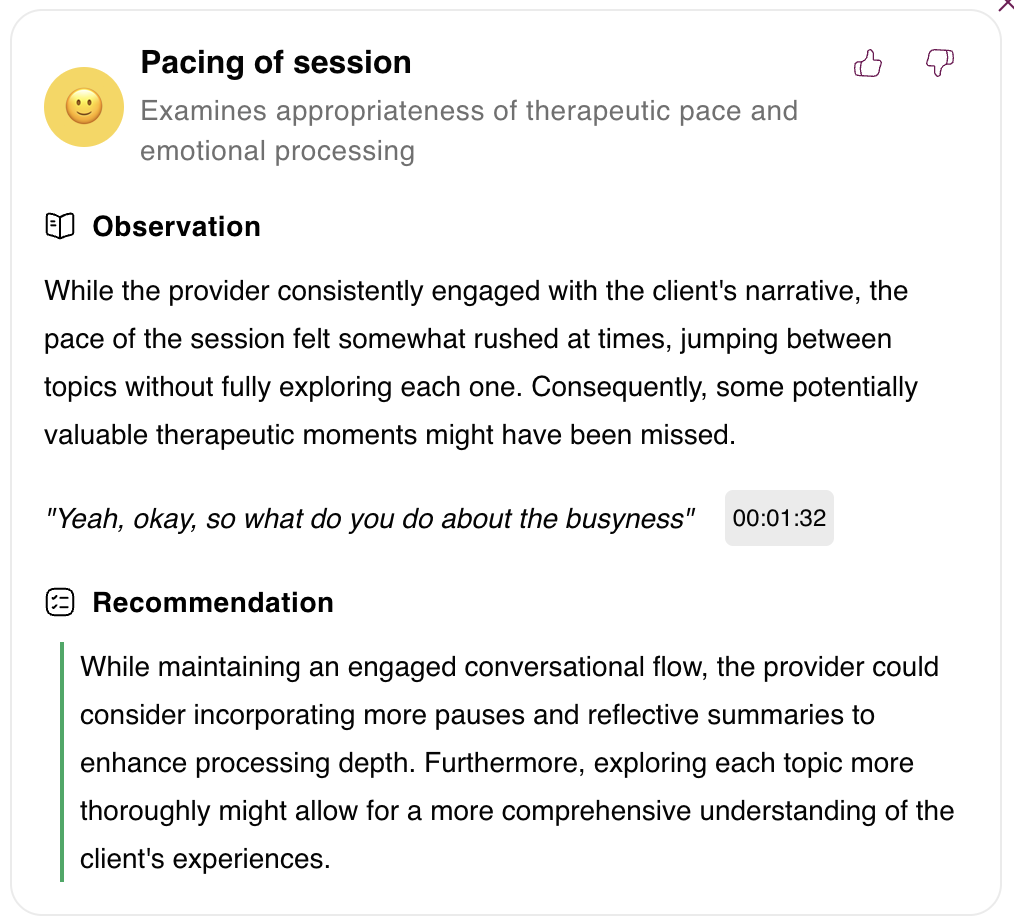
And here’s where Mentalyc – note taking tool that really makes life easier. You don’t have to struggle to find the “right words” for your notes. The platform automatically turns what you say in a session into clear, professional language that sounds exactly how progress notes should. No more stopping to figure out how to phrase things clinically — Mentalyc does that for you. This makes your notes faster, easier, and more accurate, while giving you peace of mind that they’ll meet clinical and compliance standards.
Counselor’s Thesaurus: Clinical Words to Use in Progress Notes (Describe Affect, Behavior, Cognition, and Orientation)
The Counselor’s Thesaurus represents a comprehensive compendium of lexicon and eloquent alternatives, meticulously curated to facilitate the discerning clinician in unearthing the precise verbiage that is in “finding the right words” for mental health note-taking.
Clinical Words to Describe Affect (Mood or Disposition) in Therapy Progress Notes:
These are words that describe the patient’s underlying experience of emotion or mood, such as: PLACID, PEACEFUL, RESTFUL, TRANQUIL, PREOCCUPIED, ABSORBED, ENGROSSED, LOST IN THOUGHT, PERSONABLE, FRIENDLY, PLEASANT, AFFABLE, AGREEABLE, AMIABLE, PASSIVE, INACTIVE, INERT, UNRESISTANT, ENTHUSIASTIC, ENTHUSED, ARDENT, ZEALOUS, TEARFUL, WEEPY, TEARY, DEPRESSED, DEJECTED, DISPIRITED, DISHEARTENED, CONTROLLED, DETERMINED, REGIMENTED, DISCIPLINED, FLAT, SHALLOW, DULL, SPIRITLESS, BLUNTED, CURT, ABRUPT, BRUSQUE, DETACHED, INDIFFERENT, IMPERSONAL, EUPHORIC, BOUYANT, ELATED, JOYFUL, JOVIAL, MARRY, LIGHTHEARTED, CAREFREE, CHEERFUL, HEARTY, OPTIMISTIC, SMILING, PLACID, QUIET, SOBER, SEDATE, SERIOUS, HOPELESS, DESPERATE…
Using these words to describe patient affect and mood can significantly improve clarity and precision in your notes.
Clinical Words to Describe Behavior:
RECKLESS, IRRESPONSIBLE, RASH, IMPRUDENT, IMPETUOUS, IMPULSIVE, EXCITABLE, ROUSING, HASTY, HURRIED, ABRUPT, UNEXPECTANT, RESTLESS, UNEASY, SPONTANEOUS, SELF-POSSESSED, OVER-CAUTIOUS, SLUGGISH, LETHARGIC, ORGANIZED…
Clinical Words to Describe Cognition (Thought Process):
These refer to both conscious and unconscious processes used to accumulate knowledge such as perceiving, recognizing, conceiving, and reasoning. Examples of words that can be included in your notes: JUDGEMENT, PROBLEM-SOLVING, DECISION MAKING, GOAL SETTING, COMPREHENSION, MEMORY…
Clinical Words to Describe Orientation in Mental Health Notes:
Orientation refers to one’s awareness of the self, the time, the place, and the person one is talking to. Some clinical words that can be used to describe orientation are: FORGETFUL, CONFUSED, DISORIENTED, ORIENTED, DISTRACTIBLE, DETACHED, DISTANT…
Clinical Words to Describe Speech in Progress Notes:
Speech can be characterized by an array of descriptors encompassing its multifaceted nature:
- Quantity of speech: This facet delves into the manner in which an individual engages in communication, encompassing traits such as being talkative, spontaneously expressive, expansively communicative, or experiencing paucity or poverty of speech, where minimal expression is observed.
- Rate of speech: This aspect pertains to the tempo at which speech is delivered, encompassing variations that range from rapid and hurried to leisurely and deliberate, or adhering to a normative cadence or experiencing a sense of pressure during speech.
- Volume (tone) of speech: This dimension relates to the auditory qualities of speech, encompassing a spectrum of attributes such as loudness, softness, monotonousness, weakness, or strength in vocal delivery.
- Fluency and rhythm of speech: This facet delves into the smoothness and rhythmic patterns present in speech, encompassing characteristics such as slurred speech, clarity, the presence of appropriately placed inflections, hesitancy, well-articulated delivery, or instances of aphasia.
More on Terminology… Applied to The SOAP Template
| SOAP Section | Examples of Clinical Words / Application |
| Subjective (S) | “Client reports feeling anxious and describes racing thoughts”; mood described as irritable |
| Objective (O) | Affect noted as flat, behavior withdrawn, speech slurred, orientation intact x3 |
| Assessment (A) | Thought process tangential, judgment impaired, risk assessment shows low suicidal ideation |
| Plan (P) | Continue CBT sessions, monitor cognitive changes, reassess mood and affect weekly |
To enhance the precision and clarity of your progress notes, it is crucial to employ a variety of clinical words that capture the nuances of a patient’s mental health condition. By incorporating effective clinical words, you can provide a comprehensive description of the patient’s symptoms, emotions, cognitive functioning, etc. in each of the four sections of the most commonly used SOAP note template. Let’s explore some SOAP note examples of how this be achieved.
Examples of Clinical Words to Use in the Subjective Section of Progress Notes:
a. Symptom Description:
Agitation: Agitation refers to a state of restlessness, increased motor activity, and difficulty sitting still. It is often associated with conditions such as anxiety, mania, or substance withdrawal. Documenting such symptoms in counseling session notes helps convey the patient’s level of psychological distress and can inform treatment decisions, such as the need for medications to address underlying anxiety or manic symptoms.
Anhedonia: Anhedonia describes the inability to experience pleasure or a diminished interest in activities that were previously enjoyable. It is commonly observed in depression or certain psychotic disorders. By noting such conditions in progress notes using the proper evidence-based therapy language, clinicians can track the patient’s response to treatment interventions and gauge the effectiveness of therapeutic strategies aimed at improving pleasure and engagement in daily activities.
Suicidal Ideation: Suicidal ideation involves thoughts or plans related to self-harm or suicide. Documenting suicidal ideation in progress notes and related signs and symptoms is of utmost importance, as it indicates a need for immediate attention and appropriate intervention to ensure patient safety. This information is vital for collaborative care and can guide treatment decisions, such as hospitalization or adjustments to medication regimens.
b. Emotion and Affect:
Euphoria: Euphoria signifies an exaggerated and elevated mood, often associated with manic episodes in bipolar disorder or substance-induced euphoria. Describing euphoria in progress notes provides insights into the patient’s emotional state and can help assess the severity of manic symptoms. It aids in treatment planning, such as considering mood stabilizers or addressing substance misuse.
Dysphoria: Dysphoria represents a profound and persistent state of sadness, dissatisfaction, or unease. It is frequently observed in depression, anxiety disorders, or personality disorders. Properly referring to dysphoria in progress notes helps clinicians assess the severity and chronicity of negative emotions, guide treatment decisions, and monitor the effectiveness of interventions aimed at improving mood and emotional well-being.
Flat Affect: Flat affect denotes a reduced range or absence of emotional expression. It is commonly seen in schizophrenia or other psychotic disorders. Properly documenting flat affect in progress notes provides valuable information about the patient’s emotional presentation, facilitating accurate diagnostic impressions and guiding treatment strategies, such as antipsychotic medications or psychosocial interventions.
c. Cognitive Functioning:
Disorganized Thinking: Disorganized thinking refers to difficulties in logical reasoning, coherence, or organization of thoughts. It is often observed in conditions such as schizophrenia or bipolar disorder with psychotic features. A proper description of disorganized thinking in progress notes helps clinicians assess the patient’s cognitive impairment, guide diagnostic evaluations, and tailor treatment interventions that target cognitive deficits.
Impaired Insight: Impaired insight indicates a lack of awareness or understanding of one’s own mental health condition. It can impede treatment adherence or decision-making abilities. Properly documenting impaired insight in progress notes helps track the patient’s level of awareness regarding their illness and informs treatment strategies aimed at promoting insight and treatment engagement.
Poor Concentration: Poor concentration describes difficulties in focusing, sustaining attention, or completing tasks. It is seen in conditions such as attention deficit/hyperactivity disorder (ADHD) or depression. Appropriately noting poor concentration in progress notes helps clinicians assess the impact of cognitive symptoms on daily functioning and guides treatment decisions, such as prescribing stimulant medications or implementing cognitive-behavioral strategies to improve attention and concentration.
Note: those are only a few examples rather than an extensive list of clinical words for progress notes.
Examples of Clinical Words to Use in the Objective Section of Progress Notes:
Elevate your clinical writing with precise and accurate language and psychotherapy documentation tips.
Vital Signs:
- Tachycardia: Rapid heart rate, often indicative of physiological stress or certain medical conditions.
- Hypotension: Low blood pressure, suggesting reduced perfusion and potential cardiovascular instability.
- Hyperthermia: Elevated body temperature, commonly associated with infection or systemic inflammation.
Physical Assessment:
- Pallor: Abnormally pale skin tone, suggesting reduced blood flow.
- Edema: Excessive accumulation of fluid in tissues, typically presenting as swelling.
- Crepitus: Audible or palpable crackling sounds or sensations, indicating the presence of gas or air in soft tissues.
Neurological Findings:
a. Level of Consciousness:
- Alert and Oriented: Fully awake, aware, and able to respond appropriately to stimuli.
- Obtunded: Reduced alertness and responsiveness, often associated with central nervous system depression.
- Comatose: Profoundly decreased level of consciousness, with no meaningful response to stimuli.
b. Reflexes:
- Hyperreflexia: Exaggerated reflex responses, potentially indicating an upper motor neuron lesion.
- Hyporeflexia: Diminished reflex responses, suggestive of a lower motor neuron dysfunction.
- Clonus: Repetitive, rhythmic contractions and relaxations of a muscle, typically seen in certain neurological conditions.
c. Behavior and Speech:
- Psychomotor Agitation: Restlessness and excessive movement, often accompanied by rapid speech, seen in conditions such as anxiety or mania.
- Psychomotor Retardation: Slowed movement and reduced responsiveness, commonly observed in depression or certain neurological disorders.
- Pressured Speech: Rapid and non-stop speech, often difficult to interrupt, characteristic of manic or hypomanic episodes.
Diagnostic Findings (Laboratory Results):
- Leukocytosis: Elevated white blood cell count, indicating an inflammatory or infectious process.
- Hyponatremia: Low sodium levels in the blood, potentially pointing to fluid imbalances or certain medical conditions.
- Hyperglycemia: High blood sugar levels, frequently associated with diabetes or stress-related conditions.
Examples of Clinical Words to Use in the Assessment and Plan Sections:
- acknowledged the client’s need for improvement in…
- allowed the client to openly express…
- asked the client to be mindful of…
- clarified the expectations for…
- collaborated on/with…
- discussed the client’s current behavior, coping skills, triggers, and treatment plan.
- encouraged the client to express/use mindfulness/make alternative behavioral choices about…
- Educate: Provide information about the patient’s diagnosis, treatment options, and self-care strategies.
- Teach: Offering guidance and skills training to enhance coping mechanisms or symptom management.
- Inform: Communicating relevant knowledge about the patient’s condition, prognosis, or potential treatment outcomes.
- Cognitive Restructuring: Employing cognitive-behavioral techniques to identify and modify negative or distorted thought patterns.
- Interpersonal Therapy: Focusing on improving interpersonal relationships and resolving conflicts to alleviate symptoms.
- Mindfulness-Based Interventions: Incorporating mindfulness practices to enhance self-awareness and reduce emotional distress.
- Validated: Affirming and acknowledging the patient’s experiences, emotions, and struggles.
- Empathized with: Demonstrating understanding and compassion towards the patient’s challenges and concerns.
- Actively Listened: Providing undivided attention and receptiveness to the patient’s thoughts, feelings, and concerns.
- Consult: Seeking advice or expertise from a specialist in a particular field related to the patient’s condition.
- Refer: Directing the patient to another healthcare professional or specialty service for further evaluation or treatment.
Final Thoughts
Excellence in documentation comes from balance. Progress notes should include both objective observations and subjective experiences. Objective details capture measurable, observable information, while subjective notes reflect the client’s unique perspective. When combined, these elements create more complete and meaningful documentation – also when working with behavioral health EHR templates. Mentalyc aligns with your goals, makes this process easier by automatically shaping your notes into clear, professional language that captures both sides of the story without extra effort on your part.
Consider the following strategies while crafting notes:
Objective Language:
- Use standardized rating scales or measurement tools to quantify symptom severity, such as the Hamilton Rating Scale for Depression or the Brief Psychiatric Rating Scale.
- Document observable behaviors, such as changes in sleep patterns, appetite, psychomotor activity, or social interaction.
- Incorporate relevant laboratory findings, imaging results, or diagnostic assessments to support clinical assessments and treatment decisions while applying psychiatric evaluation vocabulary.
Subjective Language:
- Quote the patient’s own words or descriptions of their experiences, providing insights into their subjective perspective.
- Use empathetic and validating language to acknowledge and reflect on the patient’s emotional struggles.
- Employ descriptive language or metaphors to capture the patient’s subjective experiences, facilitating a deeper understanding of their inner world.
Avoid Jargon and Stigma:
While clinical language is essential in psychiatric progress notes, it is crucial to strike a balance and avoid excessive jargon or stigmatizing terminology. Ensure that the language used is accessible and understandable to all healthcare professionals involved in the patient’s care. Avoid stigmatizing or judgmental terms that may perpetuate stereotypes or hinder effective communication. Choose language that promotes empathy, respect, and dignity for the patient.
Ask for Help:
Mentalyc provides an advanced yet easy-to-use solution that takes the hassle out of writing progress notes. With smart templates and clinical language support, it helps you capture client sessions clearly, quickly, and accurately—without the stress of figuring out how to phrase everything. Instead of getting stuck in paperwork, you can stay focused on what matters most: your clients. See the difference for yourself—start your free trial today and experience how Mentalyc can simplify documentation and give you back more time.
Taylor Gordon, Associate Professional Counselor:
“I think struggling to find the words to put the notes together was one of the biggest challenges. And really just making sure all of the points were being hit, but also just developing and increasing my personal therapeutic vocabulary. (…) I would highly recommend Mentalyc to others. I think previously it probably took me about 45 minutes just to do a note and now it probably takes me no more than 15.”
Katherine Killham, Licensed Professional Counselor:
“At the end of a, a long day of doing therapy, I find it really difficult to focus well enough to come up with the right vocabulary and to make things very clinical, um, and professional looking and sounding. So that’s one thing that’s been really helpful to me with Mentalyc.”
Karen Martin, LPC, Mental Health Counselor:
“I loved it, except for having to sound like a professional. That’s where I really struggled… Mentalyc puts that professional spin on the responses for me, but also easily conceptualizes what it is that the client is saying.”
Mentalyc AI Pricing & Plans
| Plan | Price | Key Features |
| 14-Day Free Trial | $0 | 14 days of full PROaccess, including 15 notes—no credit cardrequired. |
| Mini | USD 14.99 /month | Record in-personsessions, upload audiofiles, use voice-to-text,or type notes directly, etc |
| Basic | USD 29.99 /month | Everything in Mini, plus:Alliance Genie™ NEW!(limited access), Smart TP™ |
| Pro | USD 59.99 /month | EMDR, Play andPsychiatry modalities,100+ custom templatesincld. BIRP, PIRP,GIRP, PIE, and SIRP,Auto-computed CPTcodes |
| Super | USD 99.99 /month | Everything in Pro, plus:Group therapy notes foreach group member,Priority onboarding andsupport |
For more details, visit the pricing page on our website.
References:
Gibson, K. J., & Rhynas, S. J. (2015). The use of language in psychiatric nursing practice. Journal of Psychiatric and Mental Health Nursing, 22(2), 99-108.
American Psychological Association. (2010). Documentation in psychotherapy. American Psychologist, 65(7), 663–673.
Ward, K. D. (2006). Documentation: Charting and legal considerations for mental health professionals. Journal of Psychosocial Nursing and Mental Health Services, 44(11), 16–19.
Green, B. E., & Tuerk, P. (2014). A clinician’s guide to clinical words. Journal of Mental Health Counseling, 36(3), 240-249.
Sarmiento, I., Connell, M., & Kesten, K. (2016). Enhancing the quality of mental health progress notes: A systematic review of the literature. Journal of Psychiatric and Mental Health Nursing, 23(1), 68-80.
Frequently Asked Questions (FAQs) About Clinical Words to Use in Progress Notes
Why other mental health professionals love Mentalyc

“It’s so quick and easy to do notes now … I used to stay late two hours to finish my notes. Now it’s a breeze.”
Licensed Professional Counselor

“Having Mentalyc take away some of the work from me has allowed me to be more present when I’m in session with clients … it took a lot of pressure off.”
LPC

“By the end of the day, usually by the end of the session, I have my documentation done. I have a thorough, comprehensive note … It’s just saving me hours every week.”
CDCII

“It takes me less than 5 minutes to complete notes … it’s a huge time saver, a huge stress reliever.”
Licensed Marriage and Family Therapist







