Writing progress notes for every client session can be overwhelming and time-consuming, especially when you’re managing a full caseload. Many therapists describe dreading documentation—staying late after sessions, losing weekends to catch up, or feeling stuck trying to “sound professional” in notes meant for insurance.
Fortunately, you don’t have to do it all manually anymore. With the help of an online AI therapy progress note generator, therapists can now create accurate, compliant notes in just minutes.
Still, finding the right tool can feel confusing. With so many software options out there, it’s hard to know which one truly meets your needs. If you’re new to using this kind of tool, you might feel unsure about where to start.
That’s where we come in. In this blog, we’ll guide you through the process, introduce the best progress note generator software, and explain how it can make your documentation faster, easier, and more consistent.
What is a “progress note generator”?
A progress note generator is a software tool designed to help you write progress notes and complete other clinical documentation quickly and with ease. By leveraging AI technology and large data models, it generates accurate, compliant notes that reflect your sessions.
For clinicians, this means no more hours lost to manual typing. Instead, you can spend less time glued to your computer and more time focusing on what truly matters—providing care and achieving better outcomes for your patients.
One of the best tools designed specifically for this purpose is Mentalyc, an AI-powered platform built for therapists. In the next sections, we’ll introduce Mentalyc in more detail and show how it can make documentation faster, easier, and more compliant—so you can finally leave note anxiety behind.
AI Therapy Progress Note Generator vs. Manual Note-Taking
| Aspect | Mentalyc (AI-Powered Progress Notes) | Manual Note-Taking |
| Time Efficiency | Generates notes in seconds using automation. | Can take 10–60 minutes per session. |
| Accuracy & Consistency | Structured, standardized, reduces errors. | Varies by therapist, prone to inconsistencies. |
| Compliance | HIPAA-compliant, supports legal and insurance documentation. | Risk of incomplete or non-compliant notes. |
| Ease of Use | Simple dashboard, multiple input methods (record, dictate, upload, type). | Requires manual typing and formatting. |
| Burnout Prevention | Saves hours weekly, helps reduce therapist workload. | Increases administrative burden and stress. |
| Integration | Works alongside EHR systems with copy-paste functionality. | Limited; manual transfer needed. |
| Cost-Effectiveness | Affordable plans | Time lost to manual notes increases indirect costs. |
Why Do Therapists Need to Use Progress Notes Software?
For many therapists, progress notes are a constant source of stress. Long hours spent typing, staying late after sessions, or falling behind on documentation can quickly lead to burnout. The pressure to stay organized, meet compliance standards, and still provide quality care only adds to the weight.
Without the right support, it’s nearly impossible to keep up. That’s why a therapy note generator app can be a game-changer. Automating the most time-consuming parts of documentation helps therapists save hours each week, stay organized, and refocus their energy on what truly matters—supporting their clients.
Mentalyc Progress Note Generator Software
Mentalyc is the leading clinical documentation software for generating high-quality automated progress notes for therapists online. Designed specifically for mental health professionals, it takes the stress out of documentation by turning session details into clear, compliant notes within minutes.
Here are some of the key benefits therapists experience when using Mentalyc:
It saves therapists’ work time.
Many therapists spend anywhere from a few minutes to over an hour writing each progress note—often adding up to several hours of extra work every week. Mentalyc customers consistently report getting that time back. With Mentalyc’s progress note generator software, there’s no need to type or reformat. Simply record or upload an audio recording of the session, and a structured, accurate progress note is generated within seconds—saving you hours and letting you focus on your clients instead of your keyboard.
It is easy to use.
Ease of use is key when it comes to any online therapy note generator. That’s why Mentalyc was designed with simplicity in mind—so clinicians can generate notes quickly and effortlessly without wrestling with complicated software. The Mentalyc dashboard is clean and intuitive, with essential features like dictation, recording, and templates grouped neatly for easy access. Even those who admit they “aren’t good with technology” found it straightforward and stress-free.
It is tailored to your therapeutic approach.
Every therapist has a unique way of working, and no two clients are alike. That’s why Mentalyc goes beyond generic templates—it adapts to your therapeutic style and client population. Whether you practice CBT, DBT, ACT, psychodynamic, or an eclectic approach, the platform generates documentation that reflects your methods and interventions accurately. With Mentalyc, your notes sound like you—aligned with your approach, your clients, and the professional standards you need to meet.
It offers new updates and features.
One of the most important considerations when choosing progress note generator software is whether it can keep pace with evolving needs. The Mentalyc team is dedicated to exactly that—constantly adding new features that make therapy documentation faster, easier, and more compliant. But they don’t do this in isolation. Mentalyc’s team actively gathers feedback, talks directly with users, and conducts ongoing UX research to understand how therapists really work. This means every update is grounded in real clinical workflows, not guesswork.
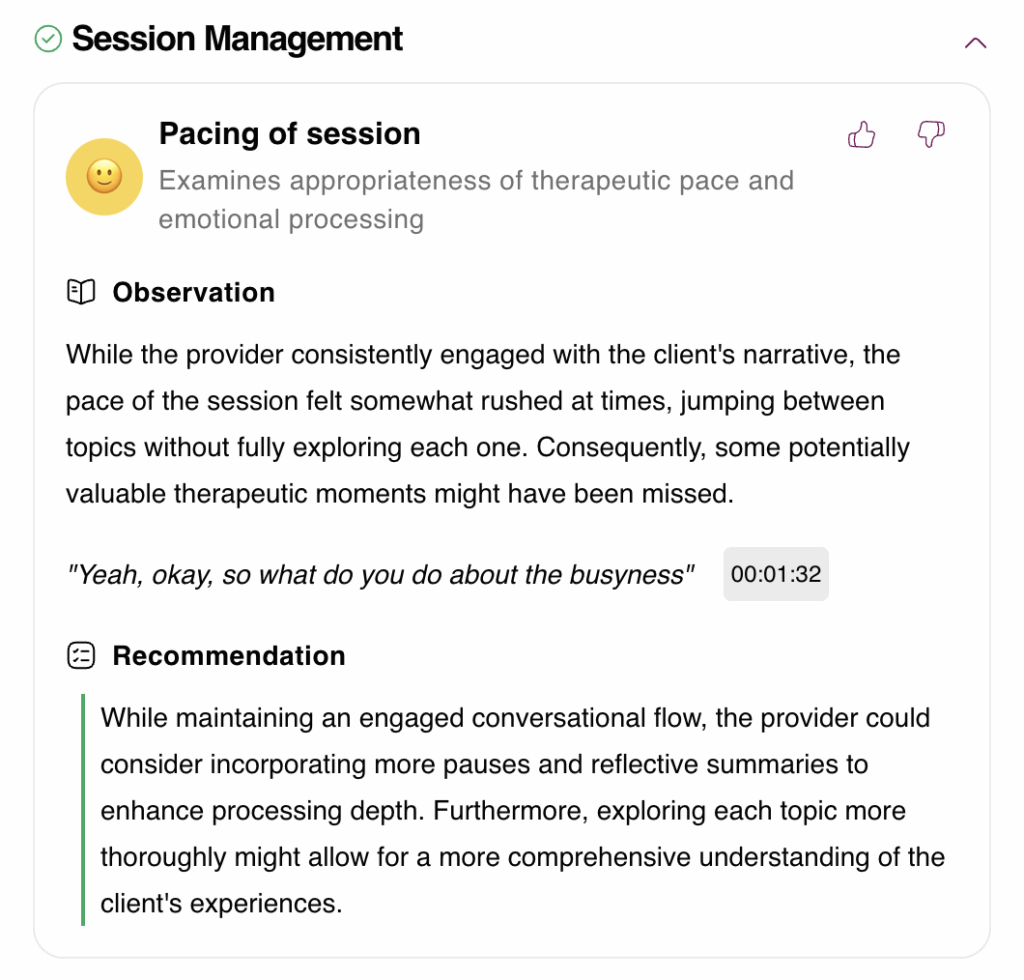
As a result, you’ll always have access to the latest improvements and tools as soon as they’re released. With this user-driven approach, Mentalyc goes beyond just automated therapy documentation—it consistently evolves to support therapists in the ways that matter most. Recent enhancements include progress tracking features, Therapeutic Alliance insights that highlight relationship strengths and blind spots after each session, and smart treatment plans that align seamlessly with progress notes and insurance requirements.
It has great support.
Before you buy any software, be sure to check what kinds of technical support are available. Otherwise, it could be a headache when you need help. We offer free technical support through phone calls and email. That way, if you have questions or run into any issues with your progress notes generator software, Mentalyc’s team is always on hand for one-on-one assistance.
It is secure.
Mentalyc is built with therapist and client confidentiality at its core. The platform is fully HIPAA-compliant and backed by a Business Associate Agreement (BAA), so you can document with confidence knowing privacy standards are met. Unlike generic note tools, Mentalyc was designed specifically for mental health care, which means your data is encrypted, protected, and never sold.
Importantly, no sensitive client information is stored beyond what’s needed for your documentation. This ensures you can use Mentalyc without hesitation—confident that your notes are secure, your practice stays compliant, and your clients’ trust is safeguarded.
It is very affordable.
Mentalyc is not only easy to use, secure, and packed with powerful features—it’s also an affordable therapy note software option. With a free trial available, you can experience how much time, stress, and energy it saves before deciding to make it part of your practice.
Step-by-Step Guide to Using Mentalyc for Progress Notes
Sign Up and Set Up Your Account
- Visit: Go to https://www.app.mentalyc.com/register and click on “Try for Free”.
- Create an Account: No credit card is required for the 14-day trial
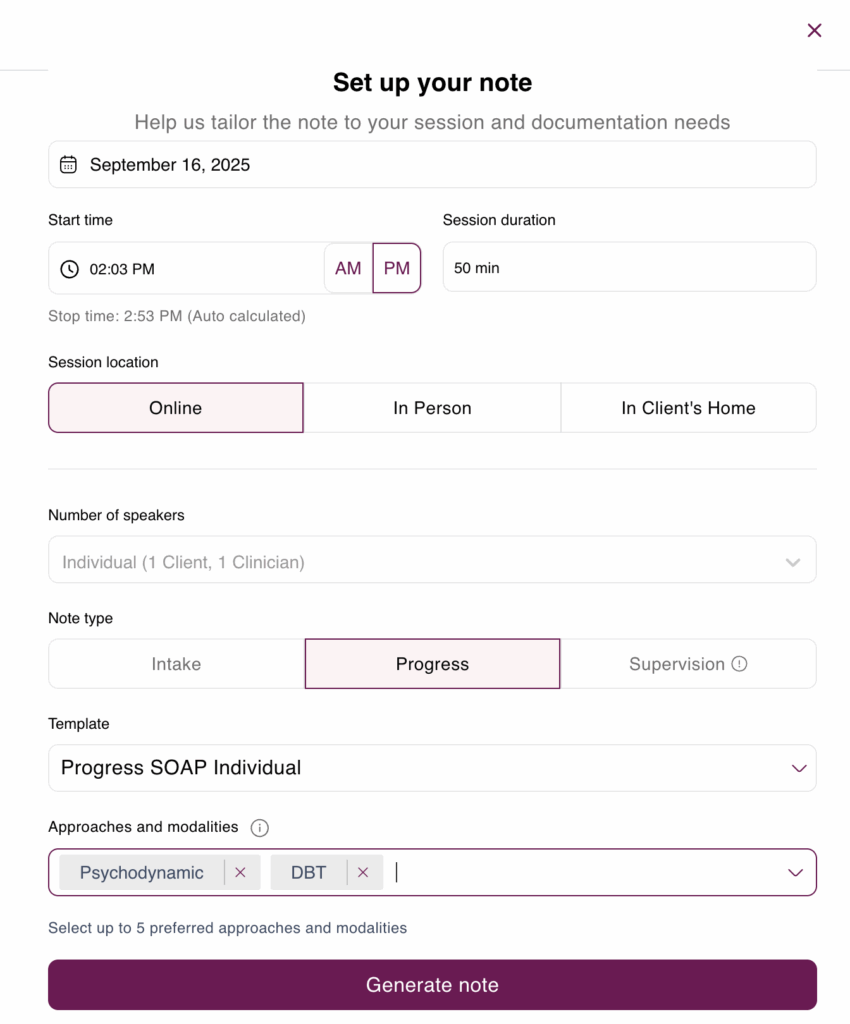
- Customize Settings: With Mentalyc’s AI mental health notes app, you can define your preferred terminology (e.g., “client” vs. “patient”), select therapy types (individual, couples, group), and choose from note formats like SOAP, DAP, or BIRP. This flexibility ensures your documentation aligns seamlessly with your practice style while maintaining compliance and consistency.
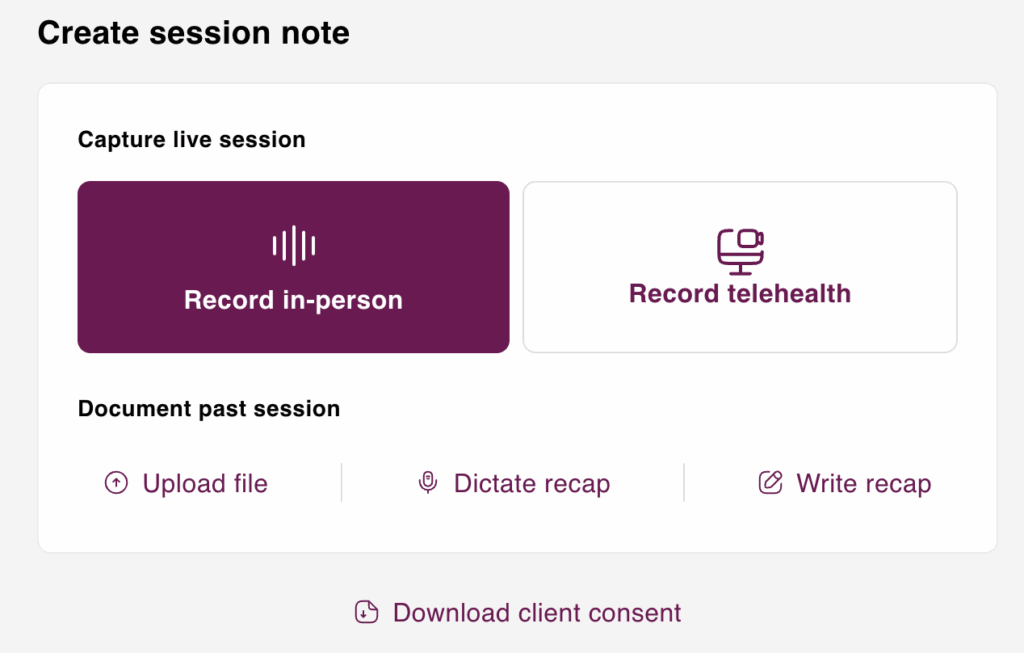
Capture Session Information
Mentalyc offers multiple input methods:
- Record Session: Use your device to record in-person or telehealth sessions.
- Dictate Recap: Verbally summarize the session if a recording isn’t available.
- Upload Audio File: Upload pre-recorded session audio.
- Describe Session: Manually enter session details or copy-paste text summaries.
These flexible options cater to various workflows and preferences.
Generate and Review AI-Created Notes
- Automatic Drafting: Mentalyc’s AI processes your input to generate structured notes within seconds.
- Note Formats: Choose from various formats like SOAP, DAP, BIRP, and more.
- Review and Edit: Quickly review the draft, make necessary edits, and approve the final version.
The AI-generated notes are crafted to be clear, structured, and fully aligned with professional documentation standards. By leveraging AI for clinical accuracy in therapy notes, you can ensure that every detail is captured correctly, reducing errors while maintaining compliance for audits, insurance, and best clinical practice.
Export and Integrate with EHR Systems
- Copy or Download: Easily copy the finalized notes or download them in your preferred format.
- EHR Integration: Mentalyc allows seamless integration with existing Electronic Health Record systems by enabling copy-paste functionality.
This ensures that your documentation is efficiently incorporated into your existing workflows.
For a visual walkthrough and further insights, consider watching the following video:
This video provides a comprehensive overview of Mentalyc’s features and demonstrates how to effectively utilize the platform for generating progress notes.
Note Types
| Format | Full Form | Description |
| SOAP | Subjective, Objective, Assessment, Plan | Widely used in healthcare; documents client-reported symptoms, observable facts, clinical assessment, and future plan. |
| DAP | Data, Assessment, Plan | Concise format focusing on session data, therapist assessment, and treatment plan. |
| BIRP | Behavior, Intervention, Response, Plan | Records client behavior, therapist intervention, client’s response, and future plan. |
| Intake Notes | Therapy Intake Notes | Summarizes client’s background, presenting issues, and initial treatment goals. |
| Customized Formats | User-defined | Therapists can tailor documentation style to align with their practice needs. |
Example of a Progress Note (Generated with Mentalyc)
Client Name: Maria Doe
Date: May 16, 2025
Session Type: Individual (Telehealth)
Therapist: Jane Jones, LCSW
Duration: 50 minutes
Subjective:
The client reported feeling “less anxious” compared to the previous week and noted improvements in her sleep. She shared that practicing breathing techniques has helped during moments of stress. However, she mentioned feeling nervous about an upcoming work presentation and described mild tension in her shoulders and chest.
Objective:
The client appeared alert and oriented. Mood was described as “better than last time.” Affect was congruent with mood. No psychomotor agitation or distress was observed. Client maintained good eye contact and was engaged throughout the session.
Assessment:
Progress noted in anxiety management and adherence to coping strategies. Client is beginning to apply learned techniques in real-life situations. Symptoms of generalized anxiety appear to be decreasing. Continued mild anticipatory anxiety about performance-related events.
Plan:
- Continue cognitive behavioral techniques to manage anxiety.
- Practice grounding strategies before stressful events.
- Explore cognitive distortions related to public speaking in the next session.
- Schedule next session for one week.
Conclusion
Progress notes are essential for continuity of care, measuring outcomes, and meeting insurance standards—but they’re also one of the biggest stressors for therapists. Many professionals describe falling behind on documentation, struggling to “sound clinical,” or sacrificing personal time just to catch up on notes.
With an AI-powered progress note generator like Mentalyc, that burden is lifted. Therapists report finishing notes right after sessions, feeling more confident in their wording, and no longer dreading paperwork.
Mentalyc functions as a true time-saving AI tool for therapists, cutting documentation hours each week while maintaining accuracy. It also supports therapy compliance and insurance documentation seamlessly—so you can stop worrying about audits and focus on providing care.
Join thousands of clinicians who already use Mentalyc to streamline their notes, stay compliant, and reclaim valuable time. Still unsure? Hear what real Mentalyc’s users are saying about how it transformed their work:
Why other mental health professionals love Mentalyc

“A lot of my clients love the functionality where I can send them a summary of what we addressed during the session, and they find it very helpful and enlightening.”
Therapist

“It immediately changed my quality of life, personally and professionally. I went from 3–4 hours a week of notes to 1 hour at most … that alone is invaluable personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (IMFT)

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“For those who have hesitations … It is a lifesaver. It will change your life and you have more time to be present with your patients.”
Licensed Clinical Social Worker
| Plan | Price | Key Features |
| 14-Day Free Trial | $0 | 14 days of full PROaccess, including 15notes—no credit cardrequired. |
| Mini | USD 14.99 /month | Record in-personsessions, upload audiofiles, use voice-to-text, or type notes directly, etc |
| Basic | USD 29.99 /month | Everything in Mini, plus:Alliance Genie™ NEW!(limited access), Smart TP™ |
| Pro | USD 59.99 /month | EMDR, Play andPsychiatry modalities,100+ custom templatesincld. BIRP, PIRP,GIRP, PIE, and SIRP,Auto-computed CPTcodes |
| Super | USD 99.99 /month | Everything in Pro, plus:Group therapy notes foreach group member,Priority onboarding andsupport |
For more information, visit the pricing page on our website.







