Therapists are required to keep detailed notes during sessions — but those notes fall under strict federal privacy laws. To stay compliant, it’s essential to understand how psychotherapy notes differ from clinical or administrative records and how to store them securely.
This guide explains what HIPAA compliance means in practice, including how to separate psychotherapy notes, protect sensitive data, and document sessions responsibly.
And while compliance starts with understanding the rules, it’s much easier to maintain with the right system. Mentalyc’s clinical intelligence platform keeps your documentation secure, structured, and fully HIPAA + SOC 2 Type II compliant — helping you protect client privacy while focusing on care.
What Makes Psychotherapy Notes HIPAA-Compliant?
To be HIPAA-compliant, your psychotherapy notes must meet specific documentation, storage, and privacy requirements. Below are the key elements that ensure your notes remain secure and compliant.

New! Transfer your notes to EHR with a single click. No more copy-pasting.
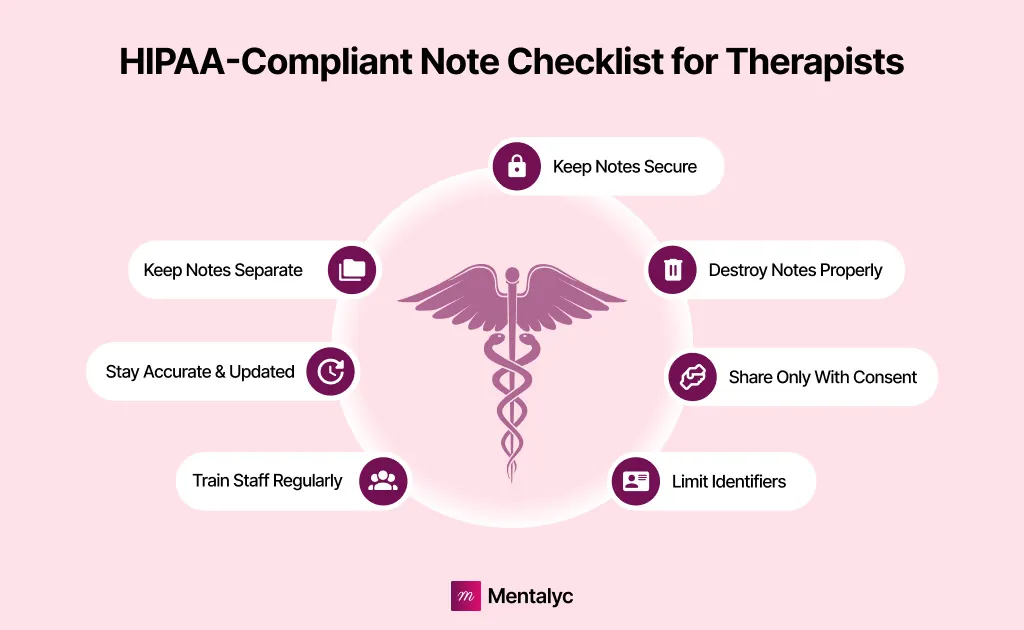
Here are the key requirements for HIPAA-compliant psychotherapy notes:
- Separate from medical records: Psychotherapy notes must be stored apart from other treatment or billing records to receive the highest level of HIPAA protection.
- Secure storage: Keep notes in a locked cabinet or encrypted, password-protected system such as a secure EHR or therapy note software.
- Access control: Only the treating therapist should have access to psychotherapy notes and administrative or billing staff should not.
- Written authorization: A client’s written consent is required before sharing psychotherapy notes, except in limited legal or safety situations.
- Limited exceptions: Therapists may review their own notes for supervision, training, or legal defense without additional consent.
- Follow state laws: Some states have stricter privacy or retention rules—always follow the most protective standard.
- Avoid clinical data: Do not include medication details, session times, diagnoses, or test results in psychotherapy notes; these belong in the medical record.
In short, HIPAA compliance means protecting client trust at every step—keeping psychotherapy notes private, secure, and separate from administrative systems.
Tip: Solutions like Mentalyc help thousand of therapists automatically separate and encrypt psychotherapy notes, reducing the risk of accidental disclosure while staying fully HIPAA-compliant.
Why HIPAA Compliance Matters in Therapy?
Under the Health Insurance Portability and Accountability Act (HIPAA), psychotherapy notes are considered protected health information (PHI). PHI is any information that could be used to identify an individual and that is related to his or her health or health care. That means therapists need to take steps to ensure that their notes are secure and that only authorized individuals have access to them.
Moreover, maintaining HIPAA compliance in therapy protects you and your clients in several ways:
- Preserves confidentiality: Protecting client data strengthens the therapeutic alliance and builds long-term trust.
- Prevents legal and financial penalties: HIPAA violations can result in fines ranging from hundreds to tens of thousands of dollars per incident.
- Protects your professional reputation: Clients and referral sources value clinicians who prioritize privacy and professionalism.
- Supports ethical documentation: Following HIPAA guidelines ensures your records meet both clinical and legal standards for accuracy, privacy, and accessibility.
Key Steps to Keep Psychotherapy Notes Secure
| Compliance Area | What to Do | Why It Matters | Best Practice Example |
| Keep Your Notes Secure | Store psychotherapy notes in a secure location such as a locked filing cabinet, password-protected computer, or HIPAA-compliant notes software. | Protects clients’ PHI (Protected Health Information) from unauthorized access or data breaches. | Use encrypted, cloud-based EHR or secure documentation platforms like Mentalyc to store and manage notes safely. |
| Keep Your Notes Separate | Store psychotherapy notes separately from the rest of a client’s medical record. | HIPAA requires separation for added confidentiality and limited disclosure. | Maintain distinct files for psychotherapy notes and progress notes; restrict access to treating providers only. |
| Be Careful With Whom You Share Notes | Share PHI only with written client authorization and disclose the minimum necessary information. | Prevents HIPAA violations and ensures ethical sharing of client data. | Before referring a client, obtain written consent and share only relevant clinical details. |
| Keep Notes Accurate and Up-to-Date | Record complete, timely, and accurate session details; correct errors by dating and initialing changes. | Accurate documentation supports continuity of care and holds up in legal or clinical review. | Review notes after each session; avoid vague language or missing context. |
| Avoid Identifying Information | Exclude personal identifiers like full names, addresses, or birthdates from psychotherapy notes. | Protects client anonymity and privacy, even within your own system. | Refer to clients as “the patient” or by initials instead of full names. |
| Destroy Old Notes Properly | Dispose of outdated notes securely through shredding, burning, or permanent data deletion. | Prevents exposure of confidential information after records are no longer needed. | Follow state-specific record retention laws before secure destruction. |
| Train Your Staff on HIPAA Compliance | Educate all staff members about HIPAA Privacy and Security Rules and your clinic’s PHI policies. | Ensures consistent protection of client information across your practice. | Conduct annual HIPAA training sessions and document staff compliance. |
Avoiding Common HIPAA Violations in Private Practice
HIPAA compliance in private practice is more than just about following checklists. It’s about building systems that protect your clients’ trust and your professional credibility. Even small oversights can lead to serious privacy breaches, fines, or reputational harm. The key is creating a workflow that makes compliance part of your daily routine, not an afterthought.
After all, compliance isn’t only about avoiding penalties. It’s a sign of respect for your clients’ vulnerability. When clients know their private information is protected, it deepens the therapeutic relationship and reinforces professional trust.
1. Understand Where Violations Happen Most
Many therapists assume HIPAA breaches occur only through major data leaks, but most violations stem from everyday habits ****like discussing client details in unsecured emails, saving notes on personal devices, or forgetting to restrict access to sensitive files. Awareness is the first line of defense: once you know where risks appear, you can design processes to prevent them.
2. Create Clear Internal Systems
Establishing structure around how you write, store, and share notes can significantly reduce risk. Separate psychotherapy notes from progress notes, set strict access levels, and create written policies on how information is stored and transmitted. When these systems are documented and reinforced regularly, compliance becomes second nature.
3. Make Security Routine, Not Reactive
Instead of waiting for an incident to reveal weaknesses, build security habits into your everyday workflow. That means regularly updating passwords, using encrypted devices, locking screens when away from your desk, and scheduling periodic audits. Small habits compound into strong data protection over time.
4. Build a Culture of Confidentiality
HIPAA compliance works best when everyone in your practice shares ownership of client privacy. Train staff, interns, or contractors on your protocols—and revisit them often. A culture of confidentiality ensures that whether you’re handling notes, emails, or consultations, everyone applies the same ethical and legal standards.
5. Stay Informed and Proactive
Regulations evolve, and so does technology. Subscribe to professional updates from the APA or HHS Office for Civil Rights to stay current on HIPAA changes. If you use digital tools, make sure your vendors renew Business Associate Agreements (BAAs) annually and continue to meet security standards.
6. Simplify Compliance With the Right Tools
HIPAA compliance doesn’t have to add to your workload. Using secure, therapist-specific platforms can help automate key parts of the process from secure storage to organized documentation.
While many tools claim to be HIPAA-compliant, not all truly meet the standard. Mentalyc actually does. As a fully HIPAA and SOC 2 Type II-compliant Clinical Intelligence platform, it keeps your psychotherapy notes separate, encrypted, and audit-ready. It ensures your data stays protected exactly as it should be.
How to Separate Psychotherapy Notes from Medical Records
One of the most common documentation mistakes therapists make is mixing psychotherapy notes with progress notes or general medical records. While both are essential for clinical care, HIPAA treats them very differently and failing to separate them can lead to privacy violations.
| Category | Psychotherapy Notes | Progress Notes |
| Purpose | Document a therapist’s personal reflections, hypotheses, or analysis from a session. Used primarily to support clinical insight and treatment planning. | Record clinical facts about treatment—session dates, interventions, progress, medications, and communication for continuity of care. |
| HIPAA Protection Level | Receive extra protection under HIPAA; not part of the medical record and cannot be shared without specific written authorization. | Considered part of the official medical record and may be shared for treatment, billing, or insurance purposes. |
| Content | Includes impressions, feelings, hypotheses, and details not meant for other providers or administrative use. | Includes diagnosis, treatment plan, medications, frequency, symptoms, and measurable client progress. |
| Access Rights | Clients generally cannot access psychotherapy notes without therapist approval, due to their sensitive nature. | Clients have the right to access progress notes as part of their health record. |
| Storage Requirements | Must be stored separately from other client records—either in a separate folder or encrypted file. | Stored within the general medical or EHR record, accessible to authorized staff. |
| Examples | Therapist’s reflection: “Client appeared defensive when discussing family conflict—possible transference noted.” | Clinical entry: “Session 4—Discussed coping strategies for anxiety; assigned relaxation exercise; client reports reduced panic frequency.” |
To remain HIPAA-compliant, you must:
- Keep psychotherapy notes in a separate, secure file so either physically in a different folder or digitally in a restricted, encrypted section of your EHR.
- Never store psychotherapy notes in the same location as progress or billing notes.
- Restrict access so only the treating therapist can view psychotherapy notes; administrative or billing staff should not have access.
- Label files clearly (e.g., “Psychotherapy Notes – Confidential”) to prevent accidental disclosure.
- Avoid quoting psychotherapy notes in documentation shared for insurance or legal purposes. Instead, summarize general themes or outcomes when necessary.
Keeping these boundaries clear not only protects your clients’ privacy but also strengthens your documentation ethics. If you’re using digital tools, choose one that allows you to store psychotherapy notes separately ****and control who can access them. That’s why most clinicians are relying on Mentalyc to document sessions securely and maintain HIPAA-compliant record separation with minimal administrative effort.
Reviewed by: Brittainy Lindsey
Disclaimer
All examples of mental health documentation are fictional and for informational purposes only.
FAQs on HIPAA-Compliant Psychotherapy Notes
How to make notes HIPAA compliant?
To make notes HIPAA compliant, store them securely (in encrypted, password-protected systems), limit access to authorized users, and avoid including unnecessary identifiers such as names or addresses. Use HIPAA-compliant note software like Mentalyc, which automatically structures and encrypts psychotherapy records, ensuring all documentation meets federal privacy and security standards.
How long should I keep psychotherapy notes?
Psychotherapy notes should generally be kept for at least 6 years after their creation, as required by HIPAA. However, state laws and licensing boards may require longer retention—often 7 to 10 years, or longer for minors. Always follow the stricter standard between HIPAA and state regulations.
What AI platforms help create psychotherapy records?
AI platforms like Mentalyc specialize in creating psychotherapy records that are accurate, HIPAA-compliant, and clinically aligned. Other general tools exist, but Mentalyc is designed specifically for therapists—it converts session summaries into structured SOAP, DAP, or progress notes while keeping client data secure and never stored.
What to include in psychotherapy notes?
Psychotherapy notes should include the therapist’s personal reflections, hypotheses, and analysis about the session—not identifying details or administrative data. Focus on the client’s emotions, themes, and your clinical impressions, keeping them separate from progress notes that document treatment goals and interventions.
Is it unethical to use ChatGPT for therapy notes?
Using public AI tools like ChatGPT for therapy notes is not HIPAA compliant and can pose ethical and legal risks if client information is shared. Instead, therapists should use HIPAA-compliant AI platforms such as Mentalyc, which securely processes information without storing sensitive data, protecting both client confidentiality and therapist liability.
What is the most common HIPAA violation?
The most common HIPAA violations include unauthorized access to patient records, sharing PHI without consent, and failing to use secure systems for storing or transmitting data. Other frequent issues involve lost or stolen devices containing unencrypted patient information.
Can a Google Form be HIPAA compliant?
A Google Form can be HIPAA compliant only if it’s created under a Google Workspace account with a signed Business Associate Agreement (BAA). The form must also use encryption, limited access permissions, and secure storage settings. Personal Gmail or free Google accounts do not meet HIPAA standards.
How much does it cost to get HIPAA compliant?
The cost of becoming HIPAA compliant varies based on practice size and systems used. Small therapy practices typically spend $1,000–$5,000 per year on compliance tools, training, and audits. Using built-in secure platforms like Mentalyc can reduce costs by combining compliance, documentation, and encryption in one place.
What’s not covered under HIPAA?
HIPAA does not cover records maintained by non-healthcare organizations, such as life insurers, employers, schools, or law enforcement agencies. It also doesn’t apply to personal health apps that operate independently from covered entities or business associates.
Why other mental health professionals love Mentalyc

“It takes me less than 5 minutes to complete notes … it’s a huge time saver, a huge stress reliever.”
Licensed Marriage and Family Therapist

“By the end of the day, usually by the end of the session, I have my documentation done. I have a thorough, comprehensive note … It’s just saving me hours every week.”
CDCII

“Having Mentalyc take away some of the work from me has allowed me to be more present when I’m in session with clients … it took a lot of pressure off.”
LPC

“It’s so quick and easy to do notes now … I used to stay late two hours to finish my notes. Now it’s a breeze.”
Licensed Professional Counselor