Crafting treatment plans for drug abuse isn’t just a paperwork exercise – it’s the backbone of effective recovery. A well-designed plan acts as a roadmap, helping clients move from ambivalence to action, and from crisis to stability. Clear, individualized planning strengthens therapeutic alliance, reduces relapse, and empowers clients to reclaim their lives.
In this blog, we’re delving into the intricacies of crafting treatment plans for drug abuse. You’ll discover why they’re indispensable, what elements they comprise, and how to implement drug abuse treatment plans effectively. Expect real-world examples, practical advice, and insider insights from clinical best practices. Ready to sharpen your skills and create plans that truly change lives? Let’s dive in.
What is a Drug Abuse Treatment Plan?
The drug abuse treatment plan is not just a roadmap but a collaborative journey toward recovery. It’s a personalized guide that includes initial assessments, tailored long-term sobriety goals, and strategies to address individual needs and circumstances. This dynamic plan is a tangible commitment to the recovery journey, fostering a shared agreement between the individual and the support team. It’s not just about the plan but the person it’s designed for.
💭 Contemplate:
- What does a personalized treatment plan look like for different clients?
- How does the flexibility of a treatment plan support long-term recovery?
Why a Drug Abuse Treatment Plan Matters in Addiction Recovery
It’s crucial to have a structured treatment plan for several reasons:
- Provides Direction: A structured treatment plan helps to maintain focus and direction, ensuring all aspects of recovery are addressed.
- Facilitates Active Participation: Involving clients in the planning process encourages them to participate actively in their recovery and empowers them to take control of their journey.
- Enhances Communication: A well-documented plan ensures that all treatment team members, including family members and other healthcare providers, are on the same page regarding the client’s progress and goals.
In short, a well-crafted treatment plan is about co-creating a path to wellness with your client and healthcare team.
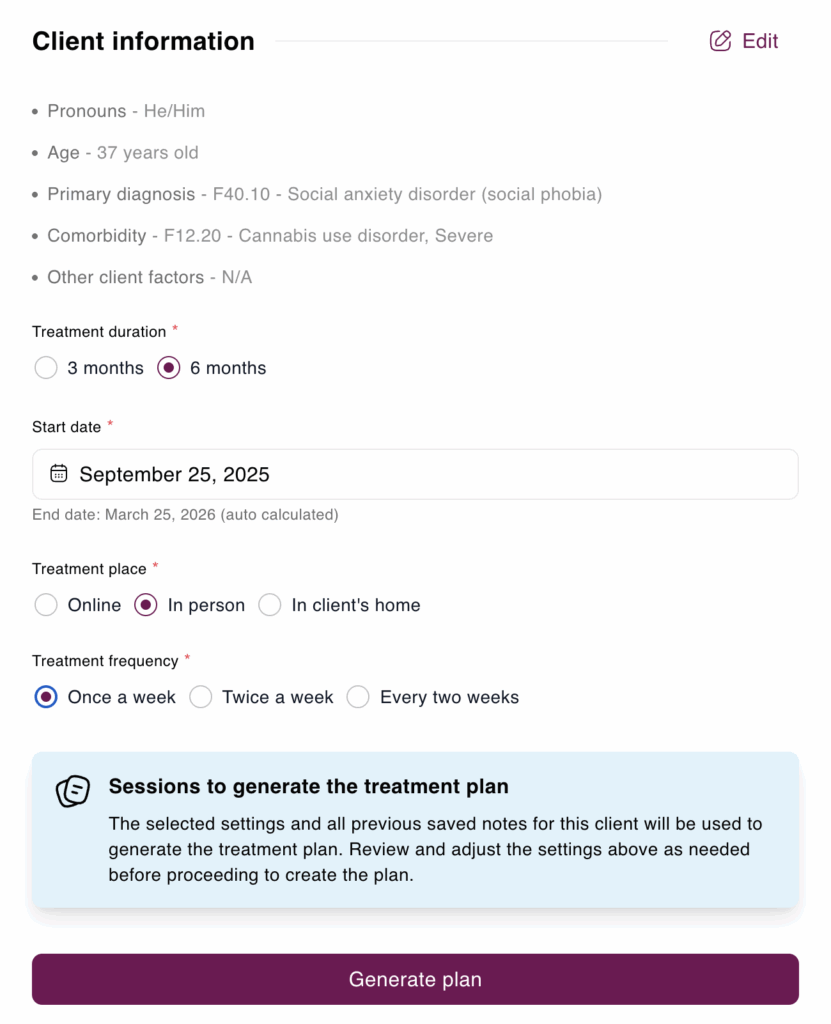
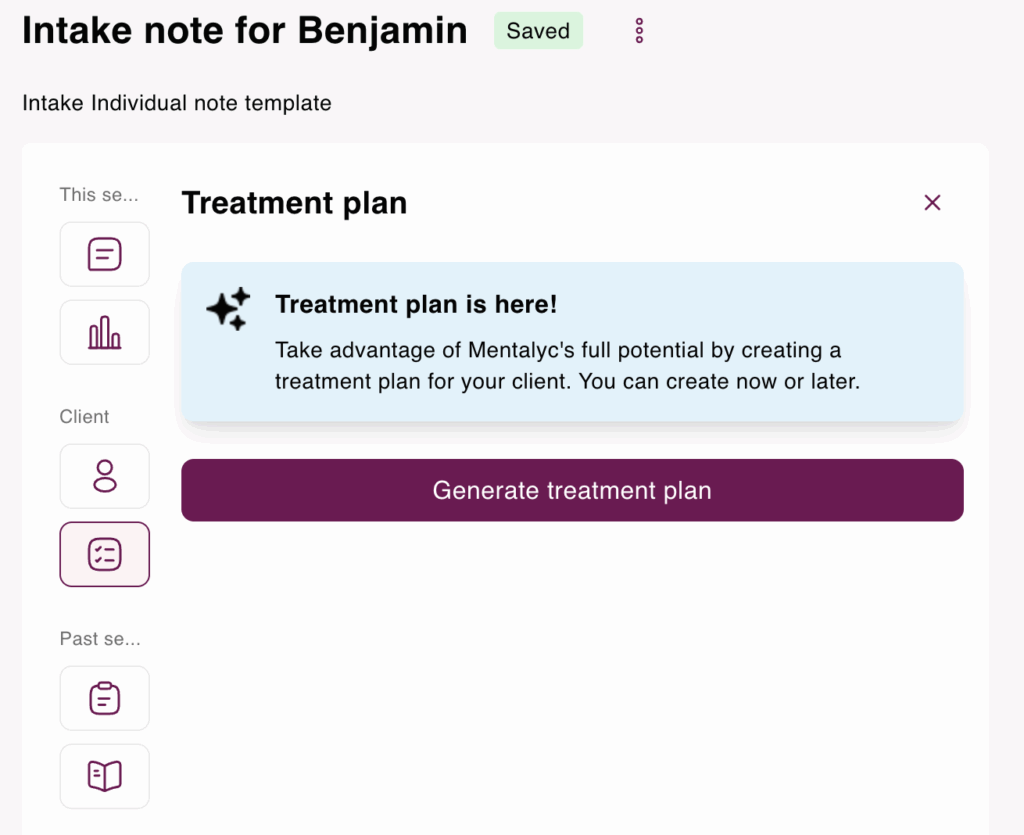
That’s where Mentalyc comes in. With its Smart TP™ feature, Mentalyc streamlines the process of creating comprehensive, insurance-ready treatment plans that are still deeply personalized. By analyzing past session data, it suggests SMART goals and interventions, that are tailored to your approach and your client’s unique needs. Each plan is automatically connected to progress notes, making it simple to track improvement over time while reducing repetitive documentation work. This not only saves hours for clinicians but also strengthens collaboration and clarity between clients, therapists, and the broader care team – ensuring treatment plans remain both clinically effective and aligned with real client progress.
Conducting a Comprehensive Drug Abuse Assessment
The first step in creating an effective treatment plan for drug addiction is to conduct a thorough assessment. This includes gathering essential information about the client’s specific situation.
Using the DSM-5 as a Guide
When assessing addiction, it’s vital to utilize the DSM-5 criteria for substance use disorders to determine the severity of the condition. By categorizing it as mild, moderate, or severe, you can establish a solid basis for our substance abuse treatment plan. A precise diagnosis allows us to set achievable objectives and select the most effective interventions.
Digging Deeper into Client History
To best support your clients, it’s essential to go beyond just identifying their diagnosis. Take the time to explore their treatment history, any co-occurring mental health conditions, and potential risk factors. This deeper understanding will enable you to create a personalized addiction treatment plan considering their unique situation. For instance, being aware of any past trauma, experiences with depression, or anxiety can influence the therapeutic interventions and approach to treatment that you choose.
Building a Complete Picture
It’s important to carefully assess all areas of the client’s life, such as their physical health, social support network, employment situation, and legal concerns. A comprehensive approach will help develop a substance use disorder treatment plan that caters to the client’s needs. By considering all aspects, we can address the underlying causes of addiction rather than just the immediate symptoms. This might involve collaborating with medical experts, social workers, and legal professionals to ensure the client receives well-rounded care.
💭 Think About:
- Why is it essential to dig deep during the assessment phase?
- How can past treatment experiences inform the current approach?
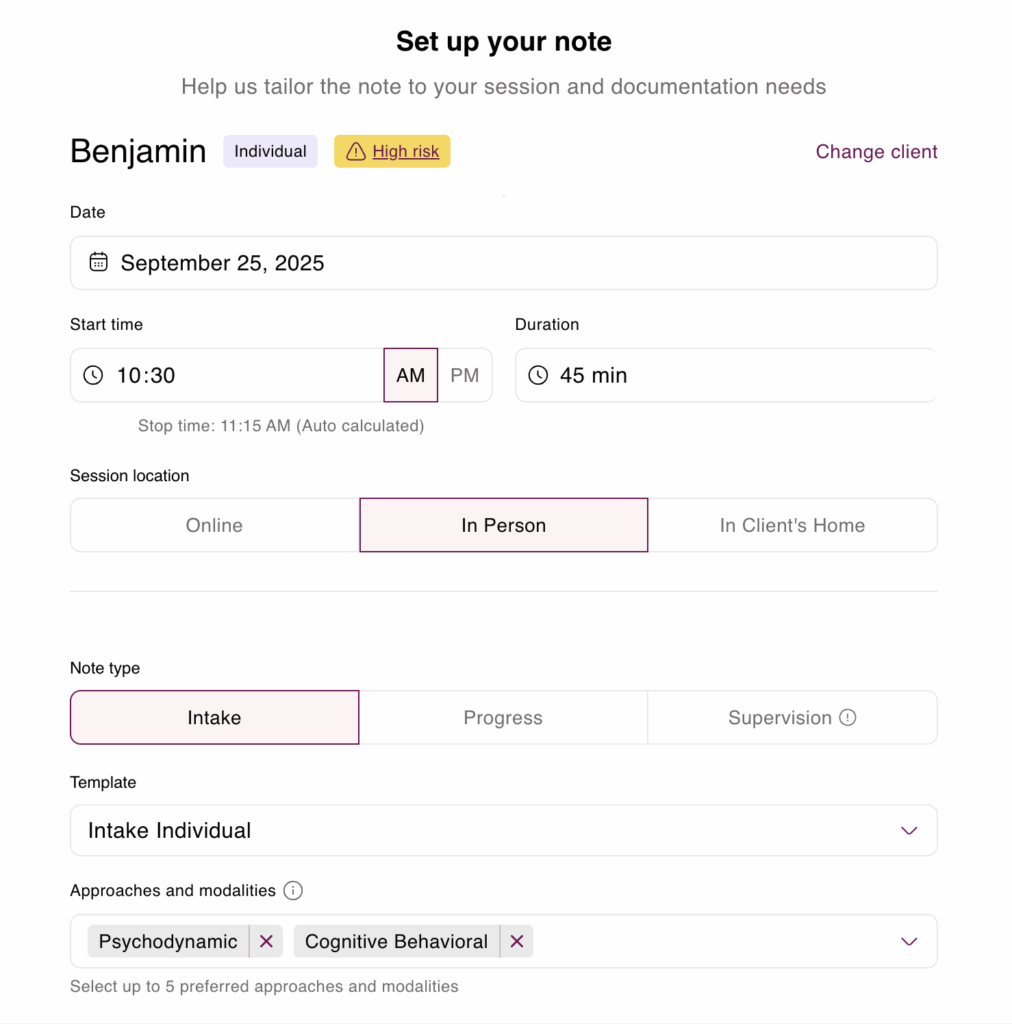
To streamline the intake process, you can use software designed to handle the heavy lifting for you. Mentalyc makes the intake and first assessment much easier. Instead of spending hours filling out forms or writing everything from scratch, the platform creates a clear draft based on what was discussed in the first sessions. It pulls in key details like the client’s main concerns, background, and any symptoms, and organizes them in a professional format that meets clinical and insurance standards. Therapists can then quickly review and adjust the draft so it truly reflects their client’s story.
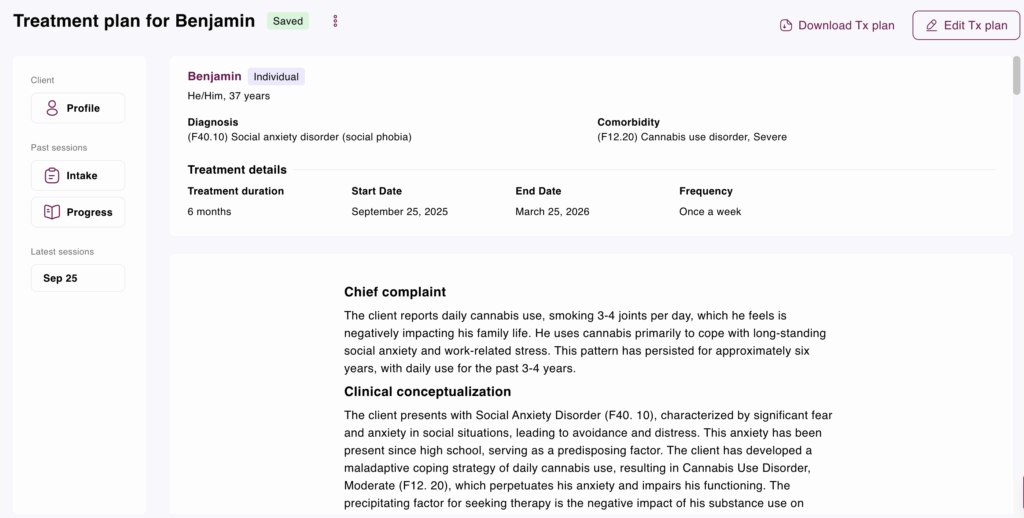
Mentalyc’s Intake Note Example for Substance Use Disorder
- Name: Benjamin
- Age: 37
- Gender: M
- Client Type: Individual
- Session date: September 25, 2025
- Start/Stop time: 10:30 AM – 11:15 AM
- Session duration: 45 minutes
- Place of service: In Person
- CPT code(s): 90791
- Diagnosis: F40.10 – Social anxiety disorder (social phobia)
- Comorbidity: F12.20 – Cannabis use disorder, Severe
Brief summary of sessionThis was an initial intake session with a new client. He presented with a chief complaint of daily cannabis use that he feels is “getting out of hand” and negatively impacting his family life. The client reports using cannabis (3-4 joints daily) for approximately six years, with daily use for the past 3-4 years, primarily to cope with long-standing social anxiety and work-related stress. He expressed a desire to reduce his use and develop healthier coping mechanisms. The session focused on gathering history, exploring the function of his substance use through a CBT lens (situation-thought-feeling-behavior cycle), and collaboratively establishing initial treatment goals. The client was receptive and insightful, agreeing with the summary of his goals. He was assigned homework to self-monitor his cannabis use and associated triggers. The clinical impression is that he meets criteria for Social Anxiety Disorder and Cannabis Use Disorder. Risk is low, and he is motivated for treatment.
Presentation
- Chief complaint: The client’s chief complaint is his daily cannabis use, which has become problematic. He smokes three to four joints per day, sometimes more, to manage long-standing social anxiety and work-related stress. He is concerned that it is negatively affecting his presence as a husband and father.
- Quote (chief complaint): “I smoke every day just to get through the anxiety, but it’s starting to run my life. My wife says I’m not really present at home, and I don’t like the kind of father I’m being when I’m always high.”
- Impairments and challenges: The client’s cannabis use and anxiety have led to impairments in several areas. Relational: His wife is frustrated, and he feels he ‘zones out’ at home, affecting his connection with her and his daughter. Occupational: He reports increased procrastination at work, despite getting his tasks done. Health/Personal: He feels ‘sluggish, forgetful, sometimes unmotivated’ and experiences guilt and paranoia after using.
- Family dynamics: The client lives with his wife and daughter. His wife has expressed worry about his cannabis use, which is a source of frustration in their relationship. The client acknowledges that his use affects his ability to be present with his daughter.
Psychological factors
- Family mental health history: NA
- Previous mental health treatments: Client reported seeing a counselor for a few sessions in college but did not continue with the treatment.
- Previous mental health assessments: NA
- Symptoms:
- Symptom 1:
- Description: The client endorses significant fear and anxiety in social situations, such as work events, meeting new people, and family gatherings. He experiences cognitive symptoms, including fear of negative evaluation (e. g. , ‘I’m going to say something dumb, ‘ ‘People will notice how awkward I am’), and physiological symptoms like getting ‘sweaty, shaky, ‘ and his mind going ‘blank. ‘ He has a history of avoiding social events due to this anxiety.
- Onset: The client reports the onset of these symptoms was in high school.
- Frequency: Symptoms are triggered by social or performance situations.
- Ascendance: This is a baseline assessment. The client describes the symptoms as a chronic, long-standing ‘theme’ throughout his life.
- Intensity: Moderate to Severe. The anxiety is intense enough to cause significant distress and has led to the development of a maladaptive coping strategy in the form of daily substance use.
- Duration: Symptoms have been present since high school.
- Symptom 2:
- Description: The client reports a problematic pattern of cannabis use, characterized by smoking every day. He uses it as a primary coping mechanism for social anxiety and work stress. This use leads to negative consequences, including guilt, paranoia, forgetfulness, and interpersonal problems with his wife. He has a persistent desire to cut down on his use.
- Onset: Casual use began approximately six years ago, escalating to a daily pattern within the last three to four years.
- Frequency: Daily. The client reports smoking ‘three or four joints’ per day, and sometimes more when stressed.
- Ascendance: This is a baseline assessment. The client reports that his use is ‘getting out of hand, ‘ suggesting an escalation in severity or negative consequences recently.
- Intensity: Moderate. The use is daily, occurs in risky situations (before work meetings), and has caused noticeable social and personal problems.
- Duration: The daily use pattern has been ongoing for the past 3-4 years.
Biological factors
- Allergies: No known allergies.
- Family medical history: Client reports that his father has hypertension and his mother has a history of depression. No known family history of substance use disorders.
- Medical conditions: Client reports feeling “sluggish, forgetful, sometimes unmotivated,” which he attributes to his cannabis use. He denies any diagnosed chronic medical conditions.
- Sleep: Reports difficulty falling asleep without cannabis; typically sleeps 5–6 hours per night, often waking feeling unrested.
- Nutrition: States appetite is variable; tends to snack heavily after evening cannabis use. Describes overall diet as “not the healthiest.”
- Physical activity: Limited; client reports minimal exercise beyond daily walking at work.
- Sexual activity: Client reports being sexually active with his wife. He notes occasional decreased libido, which he believes may be related to cannabis use and stress.
- Substances: The primary substance used is cannabis, smoked daily (3–4 joints) for the past 3–4 years. He also reports drinking alcohol socially but “not much.” He denies any history of using other illicit drugs.
Social factors
- Work or school: The client is employed and reports that he gets his work done but tends to procrastinate more than he would like. He uses cannabis to cope with work-related stress, such as deadlines, and has used it before work meetings.
- Relationships: The client is married. His relationship with his wife is strained due to his cannabis use; she is “frustrated” and notices when he is not present. He is also concerned about the impact of his use on his relationship with his daughter.
- Recreation: Client reports limited recreational activities. Most evenings are spent at home, often watching TV or playing video games after using cannabis. He notes he used to enjoy hiking but rarely engages in it now.
- Family social history: Client grew up in a two-parent household. He describes his upbringing as “mostly stable,” though communication around emotions was limited. He has one sibling with whom he maintains occasional contact.
- Cultural considerations: Client identifies as American and does not report any specific cultural or religious considerations affecting his care at this time.
- Traumatic experiences: Client denies experiencing physical or sexual abuse. He does report ongoing emotional distress during adolescence related to severe social anxiety and episodes of bullying in high school, which continue to affect his self-confidence.
- Quote (traumatic experiences):
- “I was always the shy kid, and in high school people made fun of me. I think that’s when I really started feeling like I didn’t fit in, and that feeling never really went away.”
Clinical assessment
- Clinical conceptualization: The client presents with symptoms consistent with Social Anxiety Disorder, which appears to be a long-standing issue originating in adolescence (predisposing factor). To manage the distress from this anxiety, he has developed a maladaptive coping strategy of daily cannabis use, which has now evolved into a co-occurring Cannabis Use Disorder (perpetuating factor). The precipitating factor for seeking therapy is the escalating negative impact of his substance use on his family relationships and personal functioning. Protective factors include his insight into the problem, his motivation for change, and his stated desire to be more present for his family. A CBT approach is appropriate to address the cognitive distortions fueling his social anxiety and to break the behavioral cycle of using cannabis to cope.
- Diagnoses:
- Diagnosis 1:
- Description: Social Anxiety Disorder (Social Phobia).
- DSM-5 code: 300.23
- ICD-10 code: F40.10
- Reasoning: The client reports a marked and persistent fear of social or performance situations where he might be scrutinized by others. He fears acting in a way that will be negatively evaluated (e. g. , ‘say something dumb, ‘ ‘be awkward’). These situations provoke anxiety, featuring physiological symptoms (‘sweaty, shaky, mind blank’). This pattern has persisted since high school and has led to impairment and the use of substances to cope, meeting DSM-5 criteria.
- Diagnosis 2:
- Description: Cannabis Use Disorder, Moderate.
- DSM-5 code: 304.30
- ICD-10 code: F12.20
- Reasoning: The client endorses a problematic pattern of cannabis use, including: using daily; having a persistent desire to cut down; continued use despite social/interpersonal problems (wife’s frustration); and use in situations that could be hazardous (before work meetings). The presence of these symptoms over the past year indicates a diagnosis of Cannabis Use Disorder, likely moderate in severity.
- Comorbidity: Social Anxiety Disorder (F40. 10) and Cannabis Use Disorder, Moderate (F12. 20) are comorbid. The client explicitly states that cannabis use is a primary way he copes with the symptoms of social anxiety, indicating a functional relationship between the two disorders.
- Differential diagnosis:
- Generalized Anxiety Disorder: Considered, but the client’s anxiety appears to be predominantly focused on social and performance situations rather than a wide range of topics.
- Substance-Induced Anxiety Disorder: While cannabis can induce paranoia and anxiety, the client’s social anxiety predates his daily cannabis use by many years, making a primary diagnosis of Social Anxiety Disorder more appropriate, with the substance use acting as a maintaining factor.
- Assessment tools:
- Assessment tool 1:
- Description: Clinical Interview
- Purpose: To gather information on the client’s presenting problems, history (psychosocial, medical, substance use), current functioning, and treatment goals to establish a preliminary diagnosis and treatment plan.
- Results: The clinical interview revealed symptoms consistent with Social Anxiety Disorder and Cannabis Use Disorder. The client demonstrated good insight and motivation for change.
- Status: Complete for this initial session. Further formal assessments for anxiety and substance use may be considered in the future to track progress.
Mental status exam
- Mood and affect: Mood was described as anxious and worried. Affect appeared appropriate to the content of the session, though somewhat constricted when discussing anxiety-provoking topics. Mood and affect were congruent.
- Speech and language: Speech was clear, coherent, and of a normal rate, rhythm, and volume. No language deficits were noted.
- Thought process and content: Thought process was linear and goal-directed. Thought content focused on his cannabis use, social anxiety, and impact on family. He reported anxious cognitions, such as ‘I’m going to say something dumb’ in social situations.
- Orientation: Oriented to person, place, time, and situation.
- Perceptual disturbances: The client denies hallucinations or delusions but reports occasional paranoia as a consequence of cannabis use.
- Cognition: No gross cognitive deficits were observed during the session. The client reports subjective cognitive issues, including feeling ‘forgetful’ and ‘sluggish, ‘ which he attributes to his cannabis use.
- Insight: Insight is rated as good. The client is able to recognize that his cannabis use is a problem, identify it as a coping mechanism for anxiety, and articulate the negative consequences it has on his life and relationships. He is motivated to engage in treatment.
- Risks or safety concerns: No Indication of Risk. Client denied any suicidal ideation, homicidal ideation, or self-harm behaviors.
- Hopelessness: No hopelessness reported or observed.
- Suicidal thoughts or attempts: Client denied any current or past suicidal thoughts, intent, or plans.
- Self harm: Client denied any history of non-suicidal self-injurious behavior.
- Dangerous to others: Client denied any thoughts or intent to harm others.
- Safety plan: No safety plan was initiated as no risk was identified.
Strengths and resources
- Internal strengths: The client demonstrates strong motivation for change, good insight into the connection between his anxiety and substance use, and the ability to articulate his internal experience. His concern for his family serves as a significant internal resource.
- External resources: The client is employed and has a family structure (wife and daughter) that, while strained by his substance use, provides a strong reason for him to pursue treatment.
Interventions
- Therapeutic approach or modality:
- Cognitive Behavioral Therapy (CBT).
- Psychoeducation.
- Therapeutic interventions:
- Rapport Building: Active listening and validation were used to establish a therapeutic alliance.
- Psychoeducation: The provider introduced the basic CBT model (situation, thoughts, feelings, behaviors, consequences) to help the client conceptualize the cycle of his anxiety and cannabis use.
- Collaborative Goal Setting: The provider worked with the client to summarize his presenting issues and formulate initial treatment goals, ensuring client buy-in.
- Rationale: An intake approach was used to gather essential history and build rapport. Introducing the CBT model was chosen as an initial intervention to provide the client with a framework for self-understanding and to lay the groundwork for future skills-based work, which is well-suited for both social anxiety and substance use.
Progress and response
- Response to treatment: As this was the initial session, the focus was on engagement. The client responded positively, was open in sharing his experiences, and appeared receptive to the therapeutic process. He readily agreed with the provider’s summary and the proposed plan.
- Specific examples or instances: The client actively participated in the exploration of the CBT cycle, applying it to his own experiences of social anxiety. He confirmed the accuracy of the provider’s summary by stating, ‘Yeah, thats exactly it, ‘ indicating good engagement and the formation of a collaborative alliance.
- Challenges to progress: NA
- Practitioner’s observations and reflections: The client presents as a good candidate for therapy, demonstrating high motivation and insight. The primary challenge will be addressing the deeply ingrained pattern of using cannabis to self-medicate his long-standing social anxiety. His desire to be a better husband and father appears to be a powerful catalyst for change.
Discussed goals
- Goals:
- Goal 1:
- Description: Reduce cannabis consumption from a daily to an occasional basis.
- Metrics: Progress will be tracked through client self-report on the frequency and quantity of cannabis used between sessions.
- Attainability: This goal is attainable but will be challenging and is dependent on the concurrent development of alternative coping strategies for anxiety.
- Relevance: High. This is one of the client’s primary stated goals for seeking therapy and is directly linked to improving his family relationships and personal functioning.
- Timeframe: Progress toward reduction will be reviewed weekly, with the aim of establishing a consistent decrease over the next 1-2 months.
- Goal 2:
- Description: Develop and implement non-substance-based coping strategies to manage social anxiety.
- Metrics: Progress will be measured by the client’s ability to identify anxious thoughts, challenge them, and utilize new skills (e. g. , relaxation, mindfulness) in triggering situations, as reported in session.
- Attainability: Attainable with consistent effort in and out of session.
- Relevance: High. This goal addresses the underlying driver of the client’s substance use and is critical for long-term change.
- Timeframe: This is an ongoing goal that will be a central focus throughout the course of therapy.
- Barriers to achieving goals: The primary barrier is the well-established, automatic nature of using cannabis to cope with anxiety. The severity of the underlying social anxiety will also present a significant challenge to discontinuing this coping mechanism.
Follow-up actions and plans
- Homework: The client was instructed to practice self-monitoring between sessions: specifically, to notice and be aware of the thoughts and feelings that arise immediately before he has the urge to use cannabis, without any pressure to change the behavior itself at this stage.
- Plan for future session: The plan for the next session is to review the self-monitoring homework, begin setting more specific and measurable goals for cannabis reduction, and introduce foundational CBT skills for identifying and challenging anxious thoughts.
- Plans for continued treatment: Treatment will continue with weekly sessions focused on a CBT approach to address both social anxiety and cannabis use. The short-term plan involves building self-awareness through monitoring and starting to build a toolkit of cognitive and behavioral coping skills.
- Coordination of care: NA
Setting Measurable Goals for Drug Addiction Recovery
| Category | Short-Term Goals | Long-Term Goals |
| Timeframe | Days to weeks | Months to years |
| Focus | Immediate stabilization, reduction of use, crisis management | Sustained recovery, relapse prevention, improved quality of life |
| Examples | – Attend 3 therapy sessions per week- Reduce alcohol consumption by 50% in 30 days- Begin attending NA/AA meetings | – Maintain sobriety for 1 year- Secure stable housing and employment- Rebuild relationships with family/friends |
| Purpose | Build early momentum, provide measurable progress, enhance motivation | Promote lasting behavioral change, restore functioning, support independence |
| Evaluation | Frequent monitoring and quick adjustments | Periodic reviews with focus on sustainability and relapse prevention |
Setting clear, measurable goals is the cornerstone of an effective treatment plan. The SMART framework (Specific, Measurable, Achievable, Relevant, Time-bound) allows you to define both short-term and long-term objectives. These goals provide direction and serve as milestones, boosting the individual’s confidence and motivation during the recovery process.
Short-Term vs. Long-Term Goals in Substance Abuse Treatment Plans
Differentiate between short-term goals, like attending daily therapy sessions, and long-term goals, such as maintaining sobriety for a year or rebuilding relationships with family members. Both types of goals offer direction and motivation during the recovery process. Short-term goals provide small victories that boost confidence and a sense of accomplishment, while long-term goals help the individual stay focused on the larger objectives.
Examples of SMART Goals
Here are a few examples:
- Short-Term Goal: Attend three NA meetings per week for the next month.
- Short-Term Goal: Reduce alcohol consumption by 50% within 30 days.
- Long-Term Goal: Secure stable housing within 60 days.
- Long-Term Goal: Maintain sobriety for one year, with ongoing therapy and support group attendance.
Adapting these objectives to each client’s circumstances and making necessary modifications will establish a precise path to recovery. It’s crucial to routinely review and adjust these goals to ensure they stay pertinent and attainable as the client advances, empowering you to be proactive and control the treatment process.
💭 Brainstorm:
- What challenges might you face when setting SMART goals, and how can you overcome them?
- How do short-term goals build toward long-term success?
Setting SMART goals with Mentalyc is simple and stress-free. Instead of trying to come up with perfectly worded goals on your own, the platform suggests clear options based on your session notes. These goals are already Specific, Measurable, Achievable, Relevant, and Time-bound, so they meet both clinical and insurance standards. You can easily adjust them to fit your client’s unique needs, and Mentalyc automatically connects each goal to your treatment plan and progress notes. This means you’ll always have a clear picture of how your client is moving forward – and the documentation takes care of itself.
Implementing Evidence-Based Interventions in Drug Abuse Treatment
| Intervention | Description | Primary Goals | Best Suited For |
| Cognitive Behavioral Therapy (CBT) | Helps clients identify and change unhelpful thought patterns linked to substance use. | Develop coping skills, reduce cravings, prevent relapse. | Clients with maladaptive thinking patterns or relapse triggers. |
| Motivational Interviewing (MI) | Client-centered counseling that enhances motivation for change through collaboration and empathy. | Resolve ambivalence, strengthen commitment to recovery. | Individuals uncertain or resistant to change. |
| Medication-Assisted Treatment (MAT) | Combines FDA-approved medications (e.g., methadone, buprenorphine, naltrexone) with therapy. | Manage withdrawal, reduce cravings, support long-term abstinence. | Clients with opioid or alcohol use disorders. |
For effective treatment, utilizing evidence-based interventions for substance abuse is crucial. These well-supported approaches can significantly improve the success of your treatment strategy.
Cognitive Behavioral Therapy (CBT)
CBT is an effective method for assisting individuals in recognizing and modifying harmful thought patterns associated with substance use. This form of therapy concentrates on building strategies to handle cravings and successfully navigate challenging circumstances. For example, if a client is grappling with the idea that they must consume alcohol to unwind, CBT can aid in reframing this perception and devising more positive coping strategies.
Motivational Interviewing (MI)
MI involves tapping into the client’s inner motivation to bring about change. Through open-ended questions and reflective listening, counselors can assist clients in resolving any ambivalence and reinforcing their dedication to recovery. This method is particularly effective for individuals who may initially resist change or are uncertain about the necessity of treatment. It is a collaborative process that encourages clients to actively engage in and take control of their journey toward recovery.
Medication-Assisted Treatment (MAT)
For specific individuals, integrating therapy with FDA-approved medications such as methadone, buprenorphine, or naltrexone can be a transformative approach, effectively managing withdrawal symptoms and curbing cravings. This combined treatment can be incredibly impactful for individuals dealing with opioid use disorders, offering a solid framework for sustained recovery. It’s crucial to blend medication-assisted treatment with counseling and behavioral therapies to address the psychological elements of addiction comprehensively.
💭 Consider:
- Which interventions have you found most effective, and why?
- How do you decide between different therapeutic approaches for a client?
Evaluating Progress and Adapting the Drug Abuse Treatment Plan
Recovery often involves twists and turns, so your drug abuse treatment plan must be adaptable to meet your client’s changing needs. Regularly scheduled check-ins are essential for tracking progress and identifying areas that require adjustments. Use tools like drug screens, self-reports, and client support network feedback to evaluate effectiveness.
Be ready to modify interventions and goals based on your client’s progress and any obstacles they encounter. Flexibility is crucial for maintaining client engagement and ensuring the treatment meets their evolving needs. Detailed records of these changes will help track long-term outcomes and inform future adjustments.
Lastly, remember to celebrate milestones, no matter how small—recognizing achievements, whether 30 days of sobriety or progress in rebuilding a relationship, can significantly enhance motivation and reinforce positive behaviors. These celebrations foster a sense of accomplishment and encourage continued effort.
💭 Ask Yourself:
- What signs indicate that a treatment plan needs adjustment?
- How can celebrating milestones boost a client’s motivation?
Example Treatment Plans for Drug Abuse
Let’s consider a few sample treatment plans to provide a better understanding. These plans have been carefully crafted to be thorough and personalized to meet each client’s unique needs.
Example 1: Treatment Plan for Opioid Use Disorder
- Client Information:
- Name: John Doe
- Age: 32
- Diagnosis: Severe Opioid Use Disorder, Generalized Anxiety Disorder
- History: 5-year history of opioid use, multiple unsuccessful attempts at sobriety, co-occurring anxiety.
- Assessment:
- Substance Use: Daily opioid use, primarily through prescription painkillers.
- Mental Health: Anxiety symptoms exacerbated by substance use.
- Social Support: Limited family involvement, no stable housing.
- Goals:
- Short-Term Goal: Reduce opioid use by 50% within the first 30 days.
- Long-Term Goal: Achieve and maintain opioid-free status within six months.
- Long-Term Goal: Secure stable housing within 60 days.
- Interventions:
- CBT Sessions: Weekly CBT sessions to address anxiety and develop coping strategies for managing cravings.
- MAT: Initiate buprenorphine treatment to manage withdrawal symptoms and reduce cravings.
- Support Groups: Attend three NA weekly meetings to build a support network.
- Case Management: Work with a social worker to secure stable housing and connect with community resources.
- Evaluation:
- Weekly Check-Ins: Monitor opioid use, anxiety levels, and housing progress.
- Adjustments: If opioid use does not decrease within 30 days, consider increasing MAT dosage or adding additional therapy sessions.
- Milestones:
- 30 Days: 50% reduction in opioid use.
- 60 Days: Secure stable housing.
- Six Months: Achieve opioid-free status.
Example 2: Treatment Plan for Alcohol Use Disorder
- Client Information:
- Name: Jane Smith
- Age: 45
- Diagnosis: Moderate Alcohol Use Disorder, Depression
- History: 10-year history of alcohol use, recent job loss, and marital issues.
- Assessment:
- Substance Use: Daily alcohol consumption, 6-8 drinks per day.
- Mental Health: Symptoms of depression include low mood, lack of motivation, and insomnia.
- Social Support: Strained relationships with spouse and children.
- Goals:
- Short-Term Goal: Reduce alcohol consumption by 50% within 30 days.
- Long-Term Goal: Maintain sobriety for one year.
- Long-Term Goal: Improve communication with spouse and children within 90 days.
- Interventions:
- Motivational Interviewing (MI): Weekly MI sessions to explore ambivalence toward change and reinforce commitment to sobriety.
- CBT: Weekly CBT sessions to address depressive symptoms and develop healthier coping mechanisms.
- Family Therapy: Bi-weekly family therapy sessions to improve communication and rebuild trust.
- Support Groups: Attend two AA meetings weekly to connect with others in recovery.
- Evaluation:
- Bi-weekly Check-Ins: Track alcohol consumption, mood, and family dynamics.
- Adjustments: If alcohol consumption does not decrease within 30 days, consider adding MAT or increasing the frequency of therapy sessions.
- Milestones:
- 30 Days: 50% reduction in alcohol consumption.
- 90 Days: Improved communication with spouse and children.
- One Year: Maintain sobriety.
These examples of drug abuse treatment plans illustrate how a detailed and well-structured treatment plan can guide clients’ recovery. Each plan is tailored to the individual’s unique needs and goals, offering a roadmap to overcome challenges and achieve lasting recovery.
💭 Think About:
- How do these examples compare to the plans you’ve created?
- What elements would you incorporate into your treatment planning process?
Overcoming Common Challenges
Creating and implementing a drug abuse treatment plan comes with its share of challenges. Some common obstacles to overcome include:
- Client Resistance: Motivational interviewing can effectively address ambivalence and resistance to change.
- Relapse: Including relapse prevention strategies in the treatment plan is crucial. These may involve identifying triggers, developing coping mechanisms, and having a relapse plan.
- Resource Limitations: In some cases, clients may face financial or logistical barriers to accessing treatment. Exploring community resources, sliding-scale fees, and telehealth options can make a significant difference in such cases.
To effectively support your clients as a mental health professional, it’s important to anticipate potential challenges and collaborate with them to find solutions. Maintaining flexibility, being responsive to their needs, and staying committed to the goals of the treatment plan are critical strategies for navigating these challenges.
The Takeaway
Crafting a comprehensive drug abuse treatment plan involves a delicate balance of art and science. It necessitates a profound comprehension of the individual, evidence-based interventions, and a willingness to tailor the plan. It’s essential to keep in mind that the objective is not simply achieving sobriety but also aiding the individual in constructing a rewarding, substance-free life.
By emphasizing well-defined objectives, conducting regular assessments, and employing adaptable interventions, you can develop a plan bolsters the individual’s path to recovery. It’s a joint effort that, when executed effectively, can result in long-lasting transformation and a more hopeful future for the individuals seeking assistance.
So, the next time you draft a treatment plan for drug addiction, approach it as more than administrative work. It’s a crucial support system, a roadmap, and a collaborative endeavor that could make a life-saving difference. That’s why it holds such immense significance.
Ready to elevate your treatment plans for drug abuse? Take a closer look at your current methods, apply the practical strategies in this guide, and watch the positive impact on your clients’ recovery journey. Want to go even further? Explore Mentalyc and unlock the benefits of our AI-powered progress note generator, built to save you time and strengthen your clinical work. Start today with a free trial and see how technology can enhance both your treatment plans and your clients’ outcomes.
Don’t just take our word for it – see how Mentalyc is changing the way clinicians approach treatment planning and documentation:
Mentalyc Plans & Pricing
| Plan | Price | Key Features |
| 14-Day Free Trial | $0 | 14 days of full PROaccess, including 15notes—no credit cardrequired. |
| Mini | USD 14.99 /month | Record in-personsessions, upload audio files, use voice-to-text, or type notes directly, etc |
| Basic | USD 29.99 /month | Everything in Mini, plus: AllianceGenie™NEW! (limitedaccess), Smart TP™ |
| Pro | USD 59.99 /month | EMDR, Play andPsychiatry modalities,100+ customtemplatesincld. BIRP, PIRP,GIRP, PIE, and SIRP,Auto-computed CPTcodes |
| Super | USD 99.99 /month | Everything in Pro,plus: Group therapynotes for each groupmember, Priorityonboarding andsupport |
For more information, visit the pricing page on our website.
FAQ: Your Top Questions on Drug Abuse Treatment Plans
Resources:
- Integrative Life Center. (2022, May 11).Identifying the Most Effective Treatment Plan for Substance Abuse. https://integrativelifecenter.com/substance-abuse/identifying-the-most-effective-treatment-plan-for-substance-abuse/
- J. Flowers Health Staff. (2023, July 12).Blueprint for Recovery: The Essentials of a Substance Use Disorder Treatment Plan. https://jflowershealth.com/substance-use-disorder-treatment-plan/
- Jhanjee, S. (2014, April).Evidence-Based Psychosocial Interventions in Substance Use. National Library of Medicine. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4031575/
- Mosel, S. (2024, August 2).Evidence-Based Addiction Therapies & Treatments. Laguna Treatment Hospital. https://lagunatreatment.com/addiction-research/evidence-based-treatment-options/
- National Association of Addiction Treatment Providers. (2023, April 4).Treatment Methods & Evidence-Based Practices. https://www.naatp.org/addiction-treatment-resources/treatment-methods
- Substance Abuse and Mental Health Services Administration. (2005).Substance Abuse Treatment: For Adults in the Criminal Justice System. National Library of Medicine. https://www.ncbi.nlm.nih.gov/books/NBK572945/