Ever catch yourself thinking, “Am I doing ABA notes the right way?”
Whether you’re a Registered Behavior Technician (RBT) or another kind of therapist, you’ve probably been writing notes since your very first client. Yet most of us never received clear guidance on how to make ABA notes both efficient and meaningful for the client’s interdisciplinary team.
Maybe you feel confident in your note-taking but still sense something is missing. Or maybe documentation is the part of your day you dread the most. Either way, you’re not alone. That’s exactly why we’ve put this article together—to share practical strategies and ABA session notes templates that make the process less stressful and more effective.
Even though documentation has been part of therapy for decades, it still isn’t easy to capture what really matters—succinctly, objectively, and on time. In ABA therapy, just like across healthcare services, accurate documentation isn’t just busywork. It keeps your services properly recorded, ensures insurance companies reimburse you, and allows supervisors, auditors, and team members to confidently review your work. Most importantly, it helps your clients receive consistent, high-quality care across providers while making their progress easy to see and track.
To that end, this blog will cover the following topics:
- Overview of RBT and ABA therapy
- Importance of note-taking
- Key elements of RBT and ABA notes
- Best practices for RBT and ABA note-taking
- Common pitfalls, challenges, and solutions for crafting effective ABA session notes
- Compliance and legal considerations
- Extra tips to shine ✨
Setting the Ground: Overview of RBT and ABA therapy in Behavioral Health Documentation
Applied Behavior Analysis (ABA) is a form of therapy designed to address communication issues, motor skill deficits, and behavioral disorders. The ABA has been recognized by the American Psychological Association as an evidence-based practice after it was well supported by peer-reviewed literature as a form of treatment.
Registered Behavior Technicians (RBT) and other ABA service providers refer to ABA guidelines designed for the treatment of individuals who learn and think differently, for example, those who have been diagnosed with an autism spectrum disorder as well as those with behavioral and developmental challenges. For new practitioners, following an RBT session notes guide can be extremely helpful in ensuring accuracy and compliance.
First, it’s important to recognize that ABA notes aren’t the same as therapy progress or counseling notes. They serve a unique role in guiding treatment. In behavioral health, you’ve likely encountered terms like ABA and BCBA—but what do they really mean in practice? And more importantly, how does this shape the way treatment plans are created and documented in ABA therapy?
Applied Behavior Analysis (ABA) is a structured, evidence-based approach to understanding the principles of behavior and designing individualized interventions that support meaningful change. While it can be applied in many settings, ABA therapy is most often used to support children with autism spectrum disorder (ASD). When delivered with quality, ABA is one of the most effective treatments for ASD. Clear documentation and a well-structured therapy progress notes structure make it easier to track progress, stay consistent across providers, and ensure care is truly individualized.
Tools like Mentalyc support this process by simplifying the writing of ABA notes, helping therapists save time while still meeting both clinical and insurance requirements.
The ABA framework emphasizes the consistent use of positive reinforcement to strengthen adaptive behaviors and build functional skills in children. By focusing on reinforcing what the child does well, this approach fosters learning in a supportive way. The broader aim of ABA therapy is to equip clients with practical abilities that promote both immediate growth and long-term independence.
ABA therapy is applied across diverse settings—clinics, hospitals, schools, and homes. For example, parents may encourage their children to clear the table after meals by offering small rewards. Through this kind of structured approach, Registered Behavior Technicians and other ABA therapists can carefully analyze how environment, responses, and reinforcement interact, allowing them to promote meaningful skill development.
There exist manifold differences between ABA and BCBA therapy. An ABA therapist provides direct applied behavior analysis services to clients, implementing interventions and supporting skill development. A BCBA (Board Certified Behavior Analyst), by contrast, has advanced graduate-level training and certification that qualifies them to design individualized treatment plans, analyze behavioral data, and supervise the delivery of ABA interventions. In practice, BCBAs typically guide and oversee the work of ABA therapists to ensure fidelity and effectiveness. Importantly, neither ABA nor BCBA practice is limited to autism—both focus more broadly on understanding and modifying behavior across a variety of contexts.
Why Is Note-Taking Imperative Across-The-Board?
Not only do ABA and RBT notes provide structure for each client session, they also play a vital role in shaping effective treatment. Well-written notes support the development of actionable treatment plans, make it easier to monitor progress over time, highlight trends or emerging patterns in behavior, and ensure decisions are based on reliable data that can be shared across the interdisciplinary team. Developing skill in how to write ABA session notes effectively is therefore essential for maintaining quality care and consistent outcomes.
The notes taken during ABA therapy sessions serve several important purposes, from supporting billing claims for insurance to clearly communicating the clinical rationale for ongoing services. Over the past two decades, the field of behavior analysis has expanded rapidly, fueled by strong evidence of its effectiveness for individuals with autism spectrum disorder. With this growth has come greater recognition from both state and private insurance providers, many of whom now cover ABA-based services. Alongside this increased funding, however, are heightened documentation requirements. Session notes must therefore function as a comprehensive record—capturing billed services, demonstrating the necessity of therapy, documenting client response, ensuring coordination of care, and highlighting significant clinical events. For guidance, providers often rely on structured formats and ABA session notes examples to meet these clinical and administrative standards.
In addition, ABA and RBT notes allow for objective and measurable observations, making them a critical part of clinical documentation in ABA. For instance, if a client with narcolepsy inadvertently falls asleep during session, it would be insufficient to assume they were simply tired. Instead, documenting such events precisely—following the standards illustrated in ABA therapy session notes examples used by experienced practitioners—ensures accuracy, continuity of care, and the provision of appropriate services.
As such, taking meticulous and accurate ABA and RBT notes seems paramount across every aspect of behavior analysis practice and aligns with BCBA session note requirements.
Answering the “How-To”
RBT and ABA notes are not fundamentally different from other progress notes used by mental health clinicians, but they serve a uniquely important function in behavior analysis. While the exact format may vary by organization, ABA notes and RBT documentation typically include basic session details—such as therapist and client names, date and time, teaching strategies applied, the client’s responses, coordination of care, and the therapist’s signature. What sets them apart is their weight in the ABA service model: notes written by behavior technicians often provide supervisors and stakeholders with the only written record of services delivered that day. These notes capture both the clinical data supporting therapeutic decisions and the fidelity of programming carried out. For this reason, applying RBT ABA note-taking tips is essential to ensure accuracy, professionalism, and accountability. Careful, thoughtful documentation not only meets compliance standards but also strengthens the continuity and quality of client care.
ABA Session Note Checklist for Therapists: What should be included in ABA session notes?
| Checklist Item | Details / Notes |
| Client Full Name & Date of Birth | Essential for identification and legal compliance |
| Date of Service | Record the session date |
| Session Start & End Time | Document duration for billing and compliance |
| Location of Service | Home, clinic, school, or telehealth |
| Therapist Name & Signature | Authenticate session notes |
| Concise Session Narrative | Describe therapy activities and targeted goals |
| Behavior Observed | ABC data: Antecedent, Behavior, Consequence, frequency, duration, intensity |
| Interventions Applied | Include all strategies and their outcomes |
| Progress Toward Goals | Note success or need for adjustment |
| Materials Used | List any resources, tools, or visual aids |
| Unusual Behaviors or Incidents | Include supervisor alerts if needed |
| Coordination of Care | Communication with caregivers or interdisciplinary team |
When compared to other progress notes in psychotherapy notes, RBT and ABA notes must include imperative elements such as:
Client Identifiers
- Record the client’s full legal name and date of birth.
- These are required for accurate identification, continuity of care, and legal compliance.
Date of Service
- Document the exact calendar date of the session.
Session Start and End Time
- Note the precise start and end times. This ensures accurate service duration for billing, compliance, and clinical records.
Location of Service
- Specify where the service occurred (e.g., home, clinic, school, community, or telehealth).
Session Narrative and Goals
- Provide a clear, concise, but comprehensive summary of:
- Activities conducted,
- Skills targeted,
- Specific treatment goals addressed.
- Keep this objective and aligned with the treatment plan.
Behaviors Observed
- Record observable behavior using ABC data (Antecedent, Behavior, Consequence). Include:
- Antecedents (what triggered or set the stage),
- Behavior form (physical characteristics),
- Frequency, duration, and intensity,
- Consequences (what immediately followed).
- Place observations in the developmental/social context of the learner, which is especially important for socially impaired ABA learners.
Interventions Applied and Outcomes
- List specific ABA strategies/programs used (e.g., prompting, reinforcement, shaping).
- Indicate whether targets were met, partially met, or not met.
- Note both successes and areas requiring further focus, as this informs treatment planning.
Coordination of Care (if applicable)
- Briefly document communication with caregivers, teachers, or other providers if it occurred.
Therapist Signature
- Authenticate the note with the full legal signature of the individual rendering services.
ABA Supervision Notes for RBTs (if applicable)
- When the session is delivered by an RBT, include any BCBA supervision notes or directives relevant to that session. This ensures clinical oversight and compliance with BACB standards
Finally, a therapist must remain vigilant and avoid complacency, as each session presents unique challenges and opportunities. Therefore, additional notes on unusual patterns of behavior, new behaviors, materials used and incidents requiring the supervisor’s attention are of utmost importance to create tailored strategies for each learner. These are central to clinical documentation in behavioral health and support evidence-based practice in ABA therapy.
Top Practices and Requirements for RBT and ABA Session Note-Taking
The records of your encounter with the client and the documents produced during the process are of an enduring and legally binding nature. Therefore, it is of paramount importance that they fulfill the following criteria: readability, precision, punctuality, lucidity, brevity, comprehensiveness, and veracity.
To elaborate, your notes must be:
- Clear: avoid the use of extravagant verbiage that obfuscates the message of the sentence.
- Complete
- Accurate: When crafting session notes, RBTs must keep in mind that these notes will be a permanent record of the client’s progress, necessitating accuracy and professionalism in writing.
- Concise: be specific and avoid unnecessary details
- Timely: realistically, it is advisable to allocate approximately ten minutes for jotting down your notes for a 45-minute session. Try to complete your notes within 24-72 hours after your sessions (depending on your insurance requirements) to avoid ending up unable to remember your session’s details.
- Objective: it is imperative to complete session notes objectively and professionally by strictly disclosing facts and actual information, as opposed to incorporating subjective elements such as personal thoughts and feelings.
Here are some suggestions to enhance the professionalism of your documentation:
- Emphasize active voice: avoid verbiage that portrays you as a passive spectator. Remember that you are a competent clinician and provide a critical service. Use active verbs. For example, instead of writing “the RBT observed Sarah perform the task”, write “the RBT taught Sarah how to perform the task”.
- Improve readability: notes serve as a valuable reference tool for other healthcare professionals to retrieve information rapidly. Use headings to increase readability, particularly for lengthy notes that describe a complicated or extended session.
- Employ bulleted lists and tables judiciously in cases where they are fitting: tables are efficacious in rapidly conveying significant information.
- Solely adopt standardized abbreviations: utilizing abbreviations that are familiar to Board Certified Behavior Analysts (BCBAs) and other healthcare practitioners is okay (although not preferred). On the contrary, the application of intricate or unconventional abbreviations can confuse other practitioners.
- Proofread: despite your best efforts, errors are bound to occur. Simple grammatical mistakes detract from the professional appearance of your writing. Allocate a few minutes to review and refine your work.
- Use templates: Ready note templates can streamline documentation, foster efficiency, and provide structure while ensuring that all pertinent clinical information is captured. A range of note formats is available for intake, treatment, progress, and other records. In ABA therapy, the widely used ABA SOAP notes template is one such option. However, it is important to recognize that no universal framework exists for writing progress notes. Clinicians must choose the format that best suits their practice needs, such as SOAP notes, DAP notes, GIRP notes, BIRP notes.
This short video will surely help you learn more about ABA notes: Methods, Tips, & Tech
Comparison of ABA Note Formats (SOAP, DAP, BIRP, GIRP)
| Format | Purpose / Focus | Key Components | Best Use Case |
| SOAP Notes | Standardized clinical documentation | Subjective, Objective, Assessment, Plan | ABA therapy sessions requiring structured clinical reporting |
| DAP Notes | Focused on description & assessment | Description, Assessment, Plan | Short sessions or progress updates |
| BIRP Notes | Behavioral focus | Behavior, Intervention, Response, Plan | Sessions emphasizing behavior changes and interventions |
| GIRP Notes | Goal-oriented therapy tracking | Goal, Intervention, Response, Plan | Tracking goal mastery and skill acquisition |
ABA Notes: SOAP Template
The SOAP notes template for ABA therapy is the most widely used template in ABA therapy (among others such as DAP, GIRP, BIRP, etc.) and is comprised of four distinct components, namely the Subjective (S), Objective (O), Assessment (A), and Plan (P) sections, which together provide a comprehensive and holistic overview of the client’s progress and session, supporting thorough clinical documentation in ABA therapy.
- The Subjective (S) Section: serves as a platform for the patient to express their condition, without any measurements or objective data. The use of direct quotes from the client is necessary to ensure accuracy. Social and family history, if pertinent, may also be included. This helps distinguish objective vs subjective observations in ABA notes.
- The Objective (O) Section: presents measurable data and factual observations, including physical and psychological behavior, general appearance, and client engagement level, which is central to data collection and analysis in ABA sessions.
- The Assessment (A) Section: synthesizes the information from the subjective and objective components to evaluate the client’s progress and highlight any patterns or themes observed. This section is crucial in identifying any changes from the previous session, providing differential diagnoses for new symptoms, and explaining client responses to interventions. It also facilitates accurate behavioral intervention documentation.
- Finally, the Plan (P) Section: outlines the necessary interventions and strategies needed for the client’s continued progress, including short-term goals and medications. The section provides a reflection on the effectiveness of previous strategies and details the next course of action for upcoming sessions.
Behold, an exemplary ABA SOAP note template chronicling the therapeutic journey of a client with autism. Remember to sign your note if you are following this template:
Client Information:
Date of Birth: 01/17/2015 Date: 01/02/23 Session Time: 2 pm – 4 pm
Subjective:
The client’s caregiver reported that the child has been demonstrating an increase in noncompliant behaviors at home, such as refusal to follow instructions, aggression, and self-stimulatory behaviors. The caregiver expressed concern regarding the child’s progress in the therapy program.
Objective:
During the session, the client exhibited limited eye contact, echolalia, and stimming behaviors. The therapist observed that the client had difficulty completing tasks and following instructions, which resulted in increased frustration and aggression.
Assessment:
Based on the observed behaviors, the client’s diagnosed autism spectrum disorder, and the caregiver’s report, the therapist concluded that the client’s noncompliant behaviors may be linked to difficulty with task completion and communication deficits.
Plan:
To address the client’s difficulties, the therapist will employ the following interventions:
- Increase the use of visual supports to aid in task completion and communication.
- Implement a token economy system to increase motivation and reinforce positive behaviors.
- Increase parent training to support the implementation of interventions at home in preparation for our next session this Frid10 am0am.
Signature:
RBT Melissa
For streamlined documentation, exploring automated note-taking tools for therapists can be highly effective. With Mentalyc , therapists don’t need to start from scratch. The platform provides ready-made templates for notes and can auto-generate drafts directly from session content. This not only ensures structured and compliant documentation but also saves hours of writing time, helping clinicians focus on clients rather than paperwork.
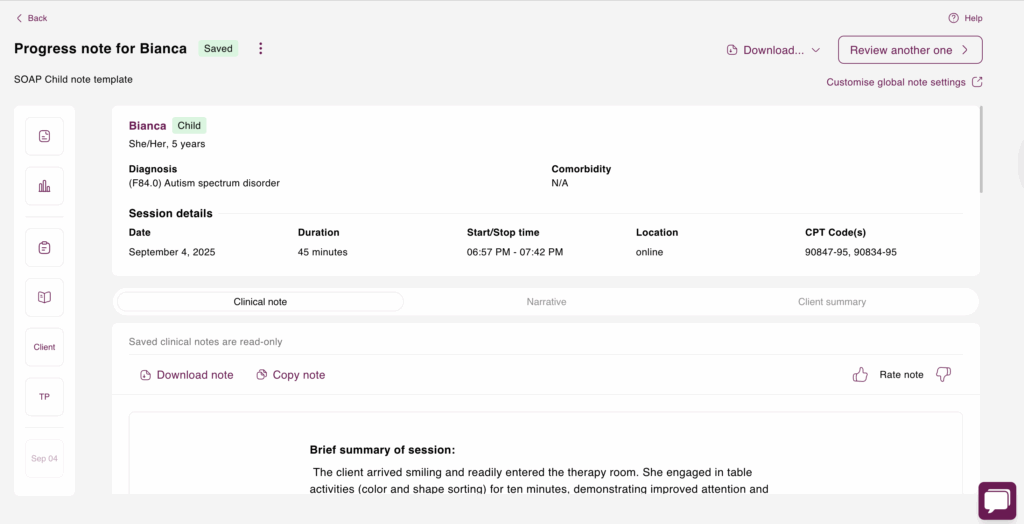
Below is a SOAP note example from an ABA session generated in Mentalyc:
Mentalyc SOAP Note Example
Subjective:
The client presented smiling and willingly entered the therapy room. While she demonstrated improved attention and readily engaged in table activities such as color and shape sorting, she required occasional reminders to remain seated. Furthermore, she independently followed two-step directions for the majority of the session and initiated play with the provider, demonstrating turn-taking skills and verbally acknowledging the provider’s turn. Although transitions presented a challenge, as evidenced by brief whining and dropping to the floor, she responded well to redirection and recovered quickly. Two specific instances of difficulty with transitions were observed, though these were shorter in duration and resolved more quickly than in previous sessions. Additionally, the client exhibited improved communication through the use of short phrases like “my turn.” Overall, progress is noted in following multi-step instructions and communicating verbally.
Objective:
A clinical interview was conducted to observe the client’s behavior, assess her progress, and plan future interventions. Play therapy was implemented to facilitate interaction and assess turn-taking skills. Redirection techniques were employed to address challenging behaviors during transitions. Positive reinforcement, utilizing praise, tokens, and access to preferred toys, was used to motivate and encourage positive behaviors. These interventions are rooted in Behavioral Therapy principles, aiming to reinforce desired behaviors and effectively manage challenging ones, while play therapy provided a context for observing and addressing social interaction and communication skills. No risks or safety concerns were identified during the session.
Assessment:
The client responded positively to the interventions, demonstrating improvements in engagement, cooperation, and communication. She showed progress in following instructions and managing transitions, specifically following two-step instructions independently most of the time, using the phrase “my turn” without prompting, and recovering quickly from brief instances of whining during transitions. While transitioning back to structured tasks presented a challenge, her overall progress towards goals is evident.
Plan:
The plan for future sessions is to continue working on two-step instructions and begin introducing three-step directions. Continued treatment will consist of Behavioral Therapy, focusing on communication, social interaction, and following multi-step instructions. No homework was assigned.
Common Pitfalls, Challenges, and Solutions for Crafting Effective ABA Session Notes
Crafting high-quality ABA notes requires time and practice. Even seasoned therapists can make common mistakes as they learn, such as employing informal and/or judgmental language.
To improve the quality of your notes, it is advisable to avoid common mistakes such as:
- Misattributing statements: Instead of using vague words such as “seemed” or “appeared,” record the exact statements as made by your client. For example, writing “the client stated he was in a good mood” is way better than writing “the client seemed to be happy”.
- Use language that conveys objective, professional observations. Avoiding certain language practices will help ensure that your notes are clear and concise, and maintain a high level of professionalism. Avoid using judgmental or opinionated language. Instead of labeling someone as “obnoxious” or “annoying”, focus on specific behaviors or actions. For example, writing “the client interrupted frequently during the session” is more informative than labeling them as “annoying”.
- Another pitfall to avoid is making subjective statements without empirical evidence. Rather than stating that “Joe was frustrated”, describe the specific observations that led you to that conclusion. Employ descriptive language that captures observable behaviors, such as “Joe slammed his fist on the table when he talked about his issues at work”.
- Refrain from using language that is vague or subjective, such as “seems” or “appears,” as this could alter the interpretation of objective observations. Instead, rely on factual and descriptive language that accurately depicts the incident, such as “the client yelled at her partner”.
- Avoid idioms and informal language. Your notes will be used by colleagues and insurance providers to evaluate your work. Hence, a formal tone is necessary.
ABA Session Notes for Insurance (Compliance and Legal Considerations)
ABA notes serve as a testament to the discerning eye of any Registered Behavior Technician, reflecting their precise observations and targeted interventions throughout therapy sessions. These notes enable clear communication among healthcare professionals, promoting continuity of care and improving treatment outcomes. More importantly, meticulous documentation substantiates the validity of insurance claims and ensures regulatory ABA session note compliance for insurance during audits.
In the context of Applied Behavior Analysis (ABA), good documentation is essential for quality care. Since clients often work with more than one therapist or healthcare provider, clear and accurate records make it possible for everyone to stay on the same page. Poor documentation can lead to confusion and gaps in care. That’s why notes must also meet legal standards—insurance companies and state regulators require them to be written carefully to ensure HIPAA and FERPA compliance in therapy records. At a minimum, your notes should include the following, in addition to any extra requirements from your state:
- Your notes should include the date, time, location, provider’s name, client’s name, and date of birth.
- Third-person writing and therapist names may be required by some insurance companies.
- The minimum elements required for compliance include patient name, date of service, type of service, start and end times, problem statement, medical necessity support, person-centered detail, patient observation, the rationale for exposure assessments, progress summary, protocols used in treatment, and coordination of treatment with other healthcare providers or service organizations.
- The patient’s name and date of service should be documented on each page of the record.
- The type of service provided, such as diagnostic assessment or group psychotherapy, should be included.
- Start and end times should also be recorded to provide a clear timeline of the therapy session.
- The problem statement should contain the diagnosis and provide context for the therapy.
- Medical necessity support should be included to justify the therapy provided and its effectiveness.
- Person-centered detail such as behavior descriptions or quotes can help illustrate the patient’s progress.
- Patient observation should be documented to note any changes in behavior or progress.
- The rationale for exposure assessments and interventions should be included, along with any safety measures taken.
- A summary of progress or lack thereof should be included, with changes to the plan of care made as necessary.
- Protocols used in treatment should be documented, along with any modifications made to them.
- Finally, coordination of treatment with other healthcare providers or service organizations should be recorded to ensure a comprehensive approach to care and facilitate ABA therapy insurance audit preparation.
Final Note: Get the Help You Need with Automated ABA Session Notes Software Like Mentalyc
Assistive services are a lifeline for ABA therapists. The role is already demanding, and the added load of endless admin can pull focus away from the heart of the work—your clients. That’s why Automated ABA session notes software, like Mentalyc, feels like such a game changer. It takes the tedious parts off your plate by generating accurate, detailed ABA notes without the grind of manual transcription.
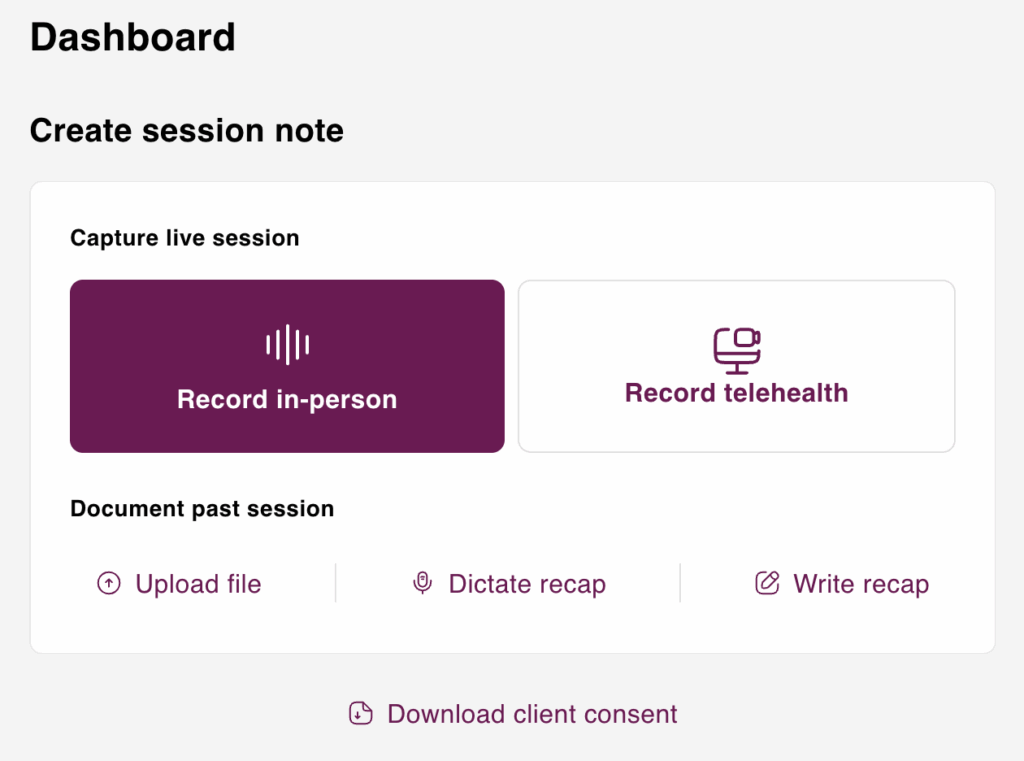
By utilizing Mentalyc, you can skip the chore of note-taking, cut down on errors, and free up your time and energy for what matters most—the therapeutic connection. And because it’s designed around session note writing best practices for therapists, you get peace of mind that your notes stay compliant while your care stays client-centered.
Clinicians explain why they recommend Mentalyc to their colleagues:
Why other mental health professionals love Mentalyc

“From treatment planning to factoring in diagnosis into the progress note, Mentalyc takes care of it all. It’s seamless.”
Licensed Clinical Social Worker

“By the end of the day, usually by the end of the session, I have my documentation done. I have a thorough, comprehensive note … It’s just saving me hours every week.”
CDCII

“If I were recommending this software to a colleague, I would tell them that it is the best thing that they could do for their practice.”
Licensed Professional Counselor

“It immediately changed my quality of life, personally and professionally.”
Owner/Independently Licensed Marriage & Family Therapist (LMFT)
Mentalyc Pricing Plans for AI Note Taking
| Plan | Price | Key Features |
| 14-Day Free Trial | $0 | 14 days of full PROaccess, including 15notes—no credit cardrequired. |
| Mini | USD 14.99 /month | Record in-personsessions, upload audiofiles, use voice-to-text,or type notes directly, etc |
| Basic | USD 29.99 /month | Everything in Mini, plus:Alliance Genie™ NEW!(limited access), Smart TP™ |
| Pro | USD 59.99 /month | EMDR, Play andPsychiatry modalities,100+ custom templatesincld. BIRP, PIRP,GIRP, PIE, and SIRP,Auto-computed CPTcodes |
| Super | USD 99.99 /month | Everything in Pro, plus:Group therapy notes for each group member,Priority onboarding andsupport |
For more details, visit the pricing page.
References
- What is applied behavior analysis? (n.d.). Child Mind Institute. Retrieved from https://childmind.org/article/what-is-applied-behavior-analysis
- Devita-Raeburn, E. (2016, August 10). The controversy over autism’s most common therapy. Spectrum News. Retrieved from https://www.spectrumnews.org/features/deep-dive/controversy-autisms-common-therapy
- Team, G. T. E. (n.d.). Applied Behavior Analysis (ABA). Applied Behavior Analysis. Retrieved from https://www.goodtherapy.org/learn-about-therapy/types/applied-behavior-therapy